Services
Podiatry
Podiatry covers any painful foot condition or mobility problem related to a foot or ankle condition, especially those complicated by conditions such as diabetes or arthritis.
Our podiatrists work to help specific problems and maintain foot health. Our orthotics service helps those who need support or correction for a physical deformity or weakness. Our teams offer a full range of advice, including taking measurements for supportive footwear where appropriate.
You can make an online referral by clicking the blue button below. If you are unable to make an online referral, please telephone 0300 421 8800 to speak to a member of our administration team, who will take your name and phone number. We will call you back at an organised time, as it will take about 10-15 minutes to complete the form.
Please note, podiatry is only able to offer a home visiting service to patients who are bedbound, who would require specialist transport to get them into a clinic. Referrals for this service can only be made by registered healthcare professionals such as GPs, nurses and other qualified staff.
Advice and information videos
Contact us
Appointments and enquiries:
0300 421 8800
Email:
podiatry.appointments@ghc.nhs.uk
The podiatry service provides high-quality expert advice and specialist treatment for conditions affecting the lower limb and foot. Our aim is to improve independence, mobility and wellbeing across all age groups.
At an initial assessment the podiatrist will agree an individual management plan for an episode of care. This involves the podiatrist and patient working together to achieve the best outcomes to improve foot problems and maintain foot health. Encouragement and support for self-care is at the centre of all that we do.
We provide a range of services to help people with every type of foot or ankle problem. If you aren’t sure which of these specialist areas is relevant, don’t worry, as we will be able to use the information you or your GP provide on the referral form to ensure you see the right person.
What is a podiatrist?
Podiatrists are Allied Health Professionals, who specialise in the assessment and management of foot and ankle conditions and associated disorders.
All podiatrists who work in our team have a minimum of a BSc in Podiatry and are HCPC registered.
A patient’s initial podiatry appointment is an assessment. This may lead to advice, a treatment plan for an episode of care or a discharge from an episode of care. Further onward referral to other specialist podiatrists or other health professionals can be completed.
Children's podiatry
Paediatric podiatrists asses lower limb structure and function. This can include concerns relating to impairment, participation and wellbeing linked to foot, ankle and lower limb health. Guidance is provided on activity, footwear, exercises and the need for orthotic/insole management; underpinned by education.
Clinics are held countywide and can be part of a multi-disciplinary setting. Referral to the service can be for any child up to the age of 18 years via a GP, Allied Health Professional or self-referral.
Diabetes
Diabetes is a long term chronic disease where the amount of glucose (sugar) in the blood is too high because the body cannot use it for energy. This is either because the body doesn’t produce enough insulin or the insulin that is being produced isn’t being used properly.
If left uncontrolled it can lead to a number of debilitating foot related complications and problems:
- Diabetic neuropathy – loss of sensation and structural change
- Vascular disease – poor healing and skin changes.
In podiatry we are concerned with the management of the moderate and high risk diabetic groups in particular. The aim is to reduce the risk of complications to the lower limb and foot, for example ulceration and amputation. This is done through regular foot checks, treatment and education.
You should see a podiatrist if you have any concerns with your feet regarding rubs, sores or ulcerations or if you feel you have any changes to your lower limb or foot, for example cramping, pain or unusual sensations.
For patients in the low risk category, your practice nurse will see you annually for a diabetic foot assessment. You do not regularly need to see a podiatrist unless you have any concerns with your foot health.
Nail surgery
Nail surgery is a commonly used procedure for the partial or total removal of problematic nail abnormalities.
Procedures are completed under a local anaesthetic with the use of phenol. The aim is to reduce the risk of a recurrence of the problem.
How to look after your feet
This service is for those individuals who have been assessed by the podiatry team and classified with an ‘at risk’, ‘moderate risk’ or ‘high risk’ foot. These patients may require intermittent or long term podiatry advice and care.
Problems often result from a combination of:
- Foot deformities
- Callus and/or corns
- Poor footwear choices or fitting
- Poor vascular status
- Neuropathy
Please note that Gloucestershire Podiatry Services do not provide a nail care service for those individuals who have been classified as having a ‘minimal’ or ‘low risk’ foot.
Rheumatology
A specialist podiatrist in rheumatology can help in several ways; from assessing your feet, prescribing insoles, reducing hard painful skin, giving advice with foot-care and footwear.
If you are seeing a consultant or being treated for rheumatological disease, such as rheumatoid arthritis or psoriatic arthritis, or if you have a connective tissue disease such as lupus, and have any foot problems, we may be able to help.
Musculoskeletal podiatry
Individuals with symptomatic foot and ankle related problems, are assessed within the MSK clinics and offered an episode of care.
An episode of care may often include a combination of:
- changes to footwear, allowing appropriate insoles/orthoses to be issued
- strengthening exercises or stretching to improve flexibility
- weight loss advice
- an onward referral to other health professionals
Advanced Practitioner Podiatrists within the team are able to request x-rays and when appropriate offer steroid injection therapy.
Partnership working
We work in partnership with other departments and organisations including Gloucestershire Hospitals NHS Foundation Trust for services such as orthotics and diabetes.
Conditions and treatments
Adult-acquired flat foot (Tibialis Posterior Dysfunction)
What is it?
This is a common foot problem that leads to a flattening of the foot and pain on the inside of the ankle and arch. It affects women more than men, usually aged between 50-80 years age.
Features
- A progressive flattening of the foot
- Low arch
- Pain
- Swelling of the inside of ankle and foot
- Foot weakness
- Feeling of ‘giving way’
- Turning in of the heel
- Turning out of the ball of the foot.
What causes it?
- Age
- Body weight
- Diabetes and medications which reduce healing – e.g. oral steroids
- Foot shape and structure (pre-existing flat foot)
- Unsupportive footwear
- Trauma (severe ankle sprain or tripping)
- Family history
- Occupation and weight-bearing hobbies
- Tight leg muscles, weak arch muscles.
What is the injury process?
The development of adult-acquired flat foot is complex. The arch of a foot is required to be strong and stable, but also flexible to aid the process of walking.
The main structures involved are the Tibialis posterior tendon located on the inside of the ankle, which is responsible for a downward and inwards turning of the foot. Also the Spring Ligament, a broad, thick band of tissue passing from heel bone to the middle of the arch.
It is thought these structures become stretched by being under too much pressure – e.g. increased body weight, poor foot function and un-supportive shoes. This leads to the foot being unstable and we see the arch flattening.
During this process the soft tissues can become inflamed, as they have to work harder to support the foot. The joints also become painful from standing while they are in a poor position. These joints can also develop osteoarthritis.
Over time, the deformity worsens and develops with limited flexibility. Typically the amount of damage accumulates slowly and you will not be aware of this change. Pain only presents after this process has been occurring for a long time.
Adult-acquired flat foot is staged on the degree of positional change seen.
Stage 1: At this stage we may not see much flattening of the foot (you have a pre-existing flat foot as a child after the age of 10 years old). You are more likely to have pain on the inside of the ankle.
Stage 2: At this stage the tendon and soft tissues stretch permanently and you will see an obvious but moderate flattening of the foot. The foot is still mobile and is still able to be put in to an improved position
Stage 3– At this stage the foot becomes fixed in a flat foot position often with more severe deformity and pain may be on the inside or outside of the ankle.
How does treatment work?
Your treatment may differ depending on the stage your foot presents with.
The aim of treatment is to reduce pain and reduce worsening deformity. This is achieved by effectively reducing the load through stretched soft tissues and attempting to improve strength in the foot and ankle. This is CRUCIAL and can be done in lots of ways that can be combined together.
An insole with an arch support does this by reducing the movement of the joints when walking.
A brace can give greater stability and support and may be considered in advancing cases.
The earlier you start managing the symptoms and comply with them the better the outcomes will be.
How to manage it
With early intervention, most patients can be treated successfully without surgery.
Commonly the condition affects one foot, but it can affect both. It can be painful, or can also occur painlessly. If there is no pain, no treatment is required. Some of these measures can improve the pain and limit the changes in foot shape.
Useful advice for all patients
- Wearing a supportive lace-up boot. This is very important. Unsupportive shoes will stop you feeling better. Avoid walking barefoot or using very thin-soled shoes.
- Not wearing the right shoes and support is a common reason for failing to improve and further flat foot progression can occur.
- Reducing your weight to a normal ‘body mass index’ (BMI) by calorie-controlled diet. Normal BMI should be under 28. https://www.nhs.uk/live-well/healthy-weight/bmi-calculator/
- Using insoles can reduce the pain – insoles that tilt the heel outward and support the arch.
- A pain-relieving insole inside the shoe should not make the shoe tighter, larger shoes may be needed. It is often worth spending time trying different insole or ankle support designs to find one that works.
- Shoes and insoles will usually help about 75% of the time.
- An ankle brace can be used to further reduce movement.
- Ankle braces and foot insoles can be either readymade or custom. It is worth trying the readymade first as this is quicker.
- Exercises that deal with any muscle tightness or weaknesses may help – http://glos-care.healthandcarevideos.com/podiatry/49214
Research has shown that having tight calf muscles causes increased load to the arch of your foot. Tight calf muscles are usually due to doing a sitting job and they tighten as we age. This is why calf stretching is recommended. We also recommend strengthening of the soft tissues on the inside of the ankle to make them better and support the arch. - Changing your work or hobbies to reduce prolonged standing
- Using pain relief such as Ibuprofen or paracetamol, unless you are not able to take this medicine. Please consult with your GP or healthcare provider.
Other pain management strategies
You can benefit from other pain management strategies such as:
- Mindfulness
- PACING
- Mental Distraction
This can help you self-manage or seek support and assistance from other health professions and groups.
Do I need further treatment?
The majority of people’s symptoms are managed with the simpler measures. This is acceptable, as this carries less risk. Further measures are usually only used when you are unable to cope with the pain and other treatments are not working.
- The initial measures should be tried for 6-12 months. It is very important to ensure all simpler measures are in place before moving on. Usually at this stage X-rays, scans and other investigations may be needed.
- Image-guided steroid injection. This is often performed to a painful joint. This is a potent dose of painkilling medicine. This can be done with an ultrasound or X-ray picture to improve accuracy and efficacy. This needs 48 hour rest and can feel worse initially. After settling, this can give benefit to many patients within 6 weeks and for up to 6 months. It can be repeated up to three times. Risks include, but not limited to, pain, making your pain worse, infection, scar tissue, bone necrosis and nerve injury.
- Aircast boot and immobilisation: This measure can be used to significantly reduce the load in the foot and ankle for a period of time – usually 6 weeks. This can give it rest to help it settle. Risks include making pain worse, loss of strength, blood clots.
- Bespoke footwear: If your foot shape cannot be accommodated in shop-bought shoes, you may be referred to an orthotist for a pair to be made for you.
Surgery
Surgical management of this is fortunately infrequent. Severe cases may be operated on. This would only be considered after all measures have been tried, often trying variations of them more than once.
There are some variations of surgery for toe joints and surgeons will need to evaluate you carefully to select the right approach.
- A common approach is to cut the heel bone in two and move the lower half inwards. This helps reduce the amount the heel rolls inwards.
- Joints of the arch can be operated on and soft tissues can be repaired or tightened.
- Sometimes the tendon that moves the big toe is used to help support the arch. This will all require screws or pins to hold things together and these pins stay in permanently.
- If the foot position is very severe and the joints of the foot are worn out, the foot shape is reconstructed by fusing the major joints of the back of the foot.
- Surgery for this problem is often extensive and will require typically 6-12 months recovery.
- Risks: Making pain worse, infection, painful scar tissue, non-healing bones, poor correction, nerve damage and chronic pain syndrome.
FAQs
- I don’t like the look of my flat foot and I’m limited with shoes I can wear – why can’t I have surgery?
Surgery carries many risks and benefits, however, the risks have to be justified. Typically this is performed in scenarios of non-improvement, pain and/or significant functional loss. Sometimes after surgery appliances and supportive footwear still need to be worn. - Do I have to wear the shoes/insoles/brace all the time?
The more you wear them, the better your symptoms are likely to be. Realistically, they need to be worn at least 80% of the time. - Can I return to playing sport and longer walks/hikes?
This depends on the severity of the condition and any other health conditions you have. At the very least you will have to consider modifying how much and what you do. - Will my foot stop being flat?
No. As the foot flattens, the connective tissues stretch and joints change position. - Why is it still sore when I don’t wear the brace?
When not wearing the supportive device/footwear, your foot will return to its flatter position, which stresses the joints and tendons again. This leads to pain. It is possible to strengthen the foot with exercises, but it isn’t always possible to be totally reliant on this alone.
Ankle Osteochondral Injury/Defect (OCD)
What is it?
The ankle joint is covered by a protective layer called cartilage. This cartilage, and sometimes the bone underneath, can be injured. This is what is referred to as an ‘Osteochondral Injury/Defect’. This is generally seen following severe ankle sprain and is often diagnosed with physical examination and history taking. This can be described as a deep pain with weight bearing and with bending of the ankle. It can also feel like the ankle can lock and catch.
Features
- Pain deep in the ankle
- Minimal swelling
- History of injury (severe ankle sprain)
- Often minimal to see on X-ray.
What causes it?
It is not completely understood, but proposed that repetitive or a single traumatic event leads to the cartilage overlying the ankle joint to bruise or detach.
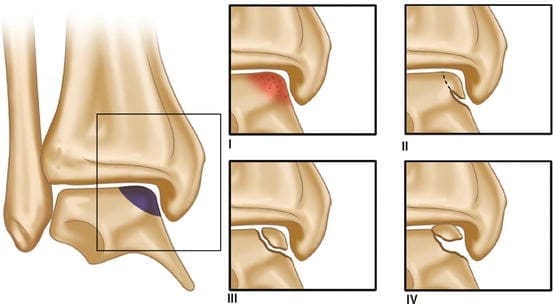
It may present with varying grades:
- Grade 1: Swelling and bone bruising
- Grade 2: Similar to grade 1, but with signs of the bone becoming loose
- Grade 3: Bone has become loose but remains in place
- Grade 4: Bone fragment completely detached
Most cases are seen with a traumatic event. However, this injury can also be seen on imaging in normal non-painful ankles, so it is important we correlate treatment with your symptoms and not the scan.
How to manage it
In early identified injury it is important to immobilise the ankle to help it heal. This can be achieved with:
- Aircast boots: An Aircast boot can be worn to significantly reduce the load on your ankle for a period of time – usually 6-12 weeks. This can give it rest to help it settle. Risks include making the pain worse, soft tissue weakening, blood clots.
- Abstaining from provoking sports for a period – rest.
- Ankle support/brace to further reduce movement. This can be either custom made or bought off the shelf, depending on the ankle.
- Changing your work or hobbies to reduce prolonged standing.
- Reducing your weight to a normal ‘body mass index’ (BMI) by calorie-controlled diet. Normal BMI should be under 28 – https://www.nhs.uk/live-well/healthy-weight/bmi-calculator
- Using pain relief such as Ibuprofen or Paracetamol unless you are not able to take this medicine. Please consult with your GP or healthcare provider.
Do I need further treatment?
Image guided steroid injection
This is a potent dose of painkilling medicine. This can be done with an ultrasound or X-ray picture to improve accuracy and efficacy. This may be used in some cases. It requires one appointment and 48 hours rest after, and often helps pain quickly. Occasionally an injection can give permanent relief. Many patients find improvement within six weeks, but return of symptoms by three months. It has risks – pain, making pain worsening, infection, skin and soft tissue thinning.
Surgery
If the above measures have failed to improve symptoms and activity is still significantly reduced, or the injury is severe, surgery is considered.
Often this is a procedure to repair or remove the cartilage fragments (arthroscopy) and (micro fracturing) to encourage blood flow back to the tissue to aid repair. This takes 6 weeks to recover from and reduced sports for up to 3 months.
Larger or more difficult-to-access lesions may need more invasive surgery and may require additional pieces of bone or cartilage to be implanted. This will require a much more lengthy recovery period.
Ankle osteoarthritis
What is it?
This is a common type of osteoarthritis (wear and tear) affecting women and men, usually aged between 50-80 years age. It can occur in one or both ankles.
Features
- Pain at rest and movement
- Joint enlargement
- Reduced movement – stiffness and unable to walk up slopes or stairs
- Malalignment – progressively ankle leaning out or in
- Heat
- Swelling
- Other foot pain due to abnormal pressure.

What causes it?
There are factors associated to its development:
- Age
- Trauma (severe ankle sprain)
- History of sporting activities
-
Family history
- Occupation and weight-bearing hobbies
- Increased bodyweight
- Foot shape and structure.
How to manage it
Ankle osteoarthritis may or may not be painful. If there is no pain, no treatment is required.
- Wearing a supportive lace-up boot
- Using insoles can reduce the pain – with a small heel raise to reduce the joint moving as much and cushioning
- A pain-relieving insole inside the shoe should not make the shoe tighter, larger shoes may be needed. It is often worth spending time trying different designs to find one that works
- Shoes and insoles will usually help about 50% of the time
- An ankle brace to further reduce movement this can be either custom made or bought off the shelf depending on the ankle
- Reducing your weight to a normal “body mass index” by calorie controlled diet normal BMI should be under 28 – https://www.nhs.uk/live-well/healthy-weight/bmi-calculator
- Exercises that deal with any muscle tightness or weaknesses may help. (http://glos-care.healthandcarevideos.com/podiatry/49214) this link needs adjusting
- Changing your work or hobbies to reduce prolonged standing
- Using pain relief such as Ibuprofen or Paracetamol unless you are not able to take this medicine. Please consult with your GP or healthcare provider.
Other pain management strategies
You can benefit from other pain management strategies such as:
- Mindfulness
- PACING
- Mental Distraction
This can be self-managed or supported with the help of other health professions and groups.
For further information visit:
- https://www.nhs.uk/conditions/osteoarthritis/
- https://www.versusarthritis.org/about-arthritis/conditions/osteoarthritis/
Will I need further treatment?
The majority of people’s symptoms are managed with the simpler measures. This is acceptable, as this carries less risk. Further measures are usually only used when you are unable to cope with the pain and other treatments are not working. These are not used solely because the ankle is very stiff or the joint is very large.
Bear in mind, pain from osteoarthritis can be episodic and can change from severe, back to mild/non-existent.
- The initial measures should be tried for 6-12 months. It is very important to ensure all the measures are in place before further treatment is considered.
- Usually at this stage X-rays and other investigations may be needed.
- Image-guided steroid injection: This is a potent dose of painkilling medicine. This can be done with an ultrasound or X-ray picture to improve accuracy and efficacy. This requires 48 hours rest and can feel worse initially. After settling, this can give benefit to many patients within 6 weeks, and for up to 6 months. It can be repeated up to three times.
- Risks include but not limited to – making your pain worse, infection, scar tissue, bone necrosis and nerve injury.
Surgery
Severe cases may require surgery. This would only be considered after all measures have been tried, often trying variations of them more than once.
There are some variations of surgery. Ankle joint osteoarthritis and surgeons will need to evaluate you carefully to select the right approach, dependent on the severity of the joint change.
- Ankle arthroscopy: This is a form of keyhole surgery to visualise bone spurs and use a burr to remove them. This is most helpful for early arthritis when the majority of the joint is still healthy and the main problem is limited movement from prominent spurs. Recovery is typically 6-8 weeks.
- In more severe cases, commonly they will look to fuse (pin together) the ankle joint so there is no movement. These pins stay in permanently. This will require 6 months recovery.
- Ankle joint replacement is occasionally performed, but much less common, as it can only be performed for a specific criteria of patients.
- Risks – making pain worse, infection, painful scar tissue, non-healing bones, poor correction, nerve damage and chronic pain syndrome.
If you are a smoker, you will be advised to stop prior to surgery. Smokers have poorer outcomes and greater risk of complications, due to nicotine levels in the body. This limits bone healing by 40%.
FAQs
- How do I walk with my ankle pinned together?
People often walk without issue after the ankle is fused. There is the perception that people will walk with an obvious limp, but this doesn’t tend to occur. The body is very good at adapting and the other ankle will mimic the pattern of the fused ankle. - Can’t you put a lubricant in the joint to preserve it?
There are injectable medicines that act as ‘lubricants’, such as hyaluronic acid. However, there is limited evidence in their effectiveness at helping osteoarthritis. Therefore, the National Institute of Clinical Excellence (NICE), that we are governed by, does not recommend their use. Other ideas are being researched such as stem cell injections – but again, there is lack of evidence for effectiveness. - Will it occur on the other ankle?
Ankle osteoarthritis is often caused from a trauma. Unlike hip osteoarthritis, which can occur without injury and through repetitive use.
Ankle sprain
What is it?
Ankle sprains are a common injury, particularly in sports populations. Eighty-five per cent are associated with ‘rolling the outside’ of the ankle.
The ankle is a very flexible joint and held together by a complex network of multiple ligaments. Ligaments are tough, short bands of tissue that connect one bone to another. On uneven ground or in other scenarios which increase the ankle’s vulnerability, the joint can rapidly move to an extreme position. This stretches the ligaments that normally give stability to the ankle. This may result in the ankle being very painful, swollen, bruised and can feel weak. This injury often improves with early intervention.

Features
- Pain
- Swelling – around the outside of the ankle primarily, sometimes top of the foot and into the leg
- Mild redness
- Limited movement in the ankle
- A feeling of instability
There are factors associated to it which may be causative:
- Uneven ground
- Unstable footwear – e.g. flexible sports shoes, high heels
- Previous history of ankle sprain
- Increased ligament laxity (hypermobility)
- Weak tendons and tight leg muscles
- Foot shape and structure
- Occupation and weight-bearing hobbies
- Bodyweight
How to manage it
Ankle sprains are graded by injury severity and treatment is tailored accordingly, with emphasis on non-surgical management. This is achieved by addressing the mechanical issues that are causing the pain and reduced function. The goal is to regain movement, strength and function in your ankle.
X-rays are used sometimes for severe sprains, but are not considered essential for the diagnoses of an ankle sprain. There are criteria that govern the use of X-ray in ankle sprains – in most cases they are not needed. X-rays are used to ensure there is no fracture or dislocation. Scans are rarely used in the first three months of the injury.
If you cannot put weight on your foot you should have an urgent assessment with your GP or Accident and Emergency Department. They will decide if you require an X-ray or other management.
Ankle ligament injuries are loosely graded based on the degree of ligament damage:
Grade 1: Milder stretching of the ligaments. Most common scenario – usually milder swelling, minimal bruising and typically able to weight bear after the injury. Usual recovery: 1-4 weeks.
This injury will usually require a short period of relative rest (24-48 hours) and then resumption of movement, with an exercise programme to strengthen the ankle.
Grade 2: A partial tearing of one or more ligaments. Less common scenario – more swelling with some bruising around the ankle bone, weight bearing may be possible, or you can be limping for a few days to a week. Usual recovery: 2-8 weeks.
This injury will usually require a period of relative rest (2-4 days) with icing and elevation to reduce pain and swelling and then gradual resumption of movement. A flexible ankle support such as a tubigrip may be helpful. Try to avoid limping or avoiding putting weight on the injury, as this stiffens it, which increases pain and slows recovery. An exercise programme is used to strengthen the ankle.
Grade 3: A full tearing of one or more ligaments. Unusual scenario – a lot of swelling and often significant bruising around the ankle, top of the foot and side of the leg. Weight bearing is usually too painful for a week or two. Usual recovery: 8-26 weeks.
This injury will need a period of rest (3-7 days). During this time some strapping may help. Ice, elevation and medicines such as Ibuprofen (after consulting your GP) will help reduce swelling and pain. Using a flexible ankle support such as an ankle stirrup can be a good idea for a few weeks. It is important to weight bear and begin moving the ankle as soon as pain and swelling will allow, to prevent it stiffening and weakening. A well-structured exercise programme is used to strengthen the ankle.
Useful advice for all patients
- Rest and ice in early presentation of sprain
- Wear supportive footwear – don’t wear loose, unstable shoes or heels
- An exercise programme that deals with the tightness or weaknesses will be beneficial. Particularly focusing on ankle stability and strengthening. Wherever possible, seek the advice of an HCPC-registered physiotherapist. Use the MSK physio referral portal or request a referral from your GP
- For ligament injuries, pain-avoidance strategies such as limping, shielding, favouring the other leg or not using a full range of movement can be unhelpful in the long run. Speak to your physiotherapist about how to both protect and strengthen the ankle.
Do I need further treatment?
- The vast majority of ankle injuries will settle within 3 months
- Residual pain following more severe sprains can persist for up to 12 months. This is because ligaments are not good at healing quickly, like other tissues.
- The measures above will usually help and 75% of sprains will clear up in 6-12 months. It is very important to ensure all the above measures are in place before moving on to further measures. Generally the research evidence is that active strengthening and balance exercises will help to improve pain and function. A large number of patients presenting with pain later on will be due to a lack of appropriate rehabilitation.
- When the condition has been bothering you for six or more months further measures will be considered. Usually at this stage imaging scans and other investigations may be considered.
- Ultrasound guided injection: This is a potent dose of pain killing medicine. As part of the healing process sometimes a ligament or joint soft-tissues can thicken due to scar tissue, which can catch in the ankle joint. This is called ‘impingement’. An injection of cortico-steroid medicine can reduce the soft-tissue inflammation associated with this and reduce pain. To ensure accuracy and efficacy this is best done with the aid of an ultrasound picture and it requires one appointment and 48 hours rest afterwards. This treatment helps most people within one month and about 50% of people by six months.
- Risks: Pain, worsening of the pain, tear of ligament, making the ankle unstable, infection, skin and soft tissue thinning, nerve injury. Often there will be a need to keep strengthening the ankle to maintain improvement.
- Ankle brace: This can be used to help stabilise the ankle and ease pain, especially in scenarios where the ankle is more vulnerable, such as partaking in sports activities or working on uneven ground. There are many available, but a lace-up or reinforced sided support is best. This should be used if the ankle is very weak, usually for 2-6 months. Risks include, making pain worse and soft tissue weakening.
Surgery
Surgery is only considered if you have not responded to at least 6 months of comprehensive conservative management, have recurrent sprains, or where pain or stiffness have a significant impact.
- The surgery may involve a ligament repair or tightening procedure. This takes 2-3 months to recover from and you may be in plaster for a period of time. There will also be a period of further rehabilitation required following this to prevent stiffening and re-injury.
- Thickened and scarred ligaments, chronically inflamed or damaged areas of the ankle joint lining that are unresponsive to other measures, such as rehabilitation and injection, can be operated on. This is typically done with keyhole surgery to trim the problem areas away. Recovery from this is 6-8 weeks.
- Risks to ankle sprain surgery include pain or worsening pain, infection, scar tissue, nerve injury and failure of repaired ligament.
FAQs
- It hurts a LOT, is this normal?
Ankle sprains are very common and therefore considered ‘ordinary’. They can be very painful and potentially incapacitating for a while. Following an exercise-based rehabilitation plan will be the best way to reduce pain and restore function. Pain avoidance and fear of movement are common – speak to a physiotherapist to be advised on how to both protect and strengthen the ankle. - Do I need a scan?
It is important to seek attention if you cannot weight bear after spraining your ankle to check for bone breaks. There are very few indications for ‘scans’ in most ankle sprains in the early stages. The vast majority of ankle sprains that don’t involve bone breaks can be graded by normal examination and will improve by following the correct rehabilitation plan. - Should I tape or bandage it?
For milder sprains this is usually not needed and can be counterproductive. Taping can also cause skin allergy or irritation. Sometimes it can be helpful in more severe injuries to support the ankle a little for a short period of time. It’s important to not make it too tight, particularly when it is swollen, and also to not limit normal ankle movement.
Chronic Plantar Fasciitis
What is it?
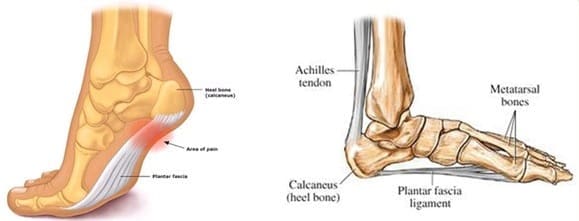
Plantar fasciitis is a pain that occurs under the heel or arch. It is a very common condition and can be very painful. It most often occurs in people aged between 40-70 years of age. It affects women and men equally. It is a chronic straining of the plantar fascia ligament. It is not a ‘spur’ or’ tear’.
Features
- Pain with first steps
- Pain improves with walking
- Pain eases with rest
- Pain with prolonged long standing/walking
- Bruised/pulling sensation.
What causes plantar fasciitis?
Its cause is not totally understood, but there are factors associated to it:
- Age
- Occupation and weight-bearing hobbies
- Bodyweight (above 28 BMI)
- Foot shape and structure
- Tight leg muscles, weak arch muscles.
What is the injury process?
It is thought that the plantar fascia becomes damaged by being stretched too much and being under too much pressure.
The plantar fascia’s function is to hold up the arch of the foot and is therefore under tension when we are standing/walking. Often the tension can increase to a level that damages the fascia – e.g. from increased body weight, or your arch has flattened over time. Sometimes the pressure on the heel can also increase because of these unhelpful loads.
Typically, the damage accumulates slowly. In the early stages, often you will not be aware of it happening with the pain only presenting after this process has been occurring for a long time.
How does treatment work?
The key to making this better is to effectively reduce the load on the plantar fascia. This is CRUCIAL and can be carried out in lots of ways that can be combined. The earlier you start managing the symptoms and comply with them, the better the outcomes will be.
How to manage it
- Reducing your weight to a normal ‘body mass index’ (BMI) by calorie-controlled diet normal. BMI should be under 28 – https://www.nhs.uk/live-well/healthy-weight/bmi-calculator/
- Avoid barefoot walking
- Wear supportive footwear at all times, such as trainers, and use insoles to reduce pain
- An insole will usually have some support under the arch to reduce the plantar fascia stretching. Also, lifting under the arch reduces pressure on the heel. Sometimes combining the arch support with a soft area, or even a hole under the most painful spot, can be helpful.
- Supportive strapping/taping: This is applied to the bottom of the foot, can provide helpful support and can be used on its own or with an insole.
- Night splints: This is a device worn at night to help stretch the calf muscles – it is not to be walked in. This can help alleviate morning pain. Please be aware that prices may vary, so shopping around may be helpful.
- Exercises that deal with any muscle tightness or weaknesses may help
- Research has shown that having tight calf muscles causes your plantar fascia to compensate and therefore stretch further than normal. Tight calf muscles usually occur from doing a sitting job and they tighten as we age. This is why calf stretching is recommended. It has been found that in patients with plantar fasciitis the muscles in the arch of the foot are smaller and weaker. Building these muscles can help reduce excessive stretching load through the fascia.
- Changing your work or hobbies to reduce prolonged standing.
- Use pain relief such as ibuprofen or paracetamol, unless you are not able to take these medicines. Please consult with your GP or healthcare provider.
The majority of patients’ symptoms resolve within 12-18 months. Engaging with treatment and self-management will reduce the pain you experience day to day. Overall, 90% of cases self-settle within 18 months. Hard-to-cure patients will typically settle in 2-3 years – it is not clear how or why this happens.
Other pain management strategies
You benefit from other pain management strategies such as:
- Mindfulness
- PACING
- Mental distraction
This can help you to self-manage or seek support and assistance from other health professions and groups.
Cortico-steroid injections and COVID-19
COVID-19 is a new viral infection in humans which has been relatively unstudied as a result. There remains a lot we do not know about the virus and, as such, it is very difficult to give firm, reliable advice to you. There are special concerns over steroid joint and soft-tissue injections and this information may help you understand this better.
Cortico-steroid, or ‘steroid’ or ‘cortisone’ injections, are pain-relieving medicines commonly used to give relief of symptoms in many joint and soft-tissue problems. Examples of where they are used are osteoarthritis, carpal tunnel, shoulder impingement and plantar fasciitis. They are very useful, as they are fast-acting, commonly superior pain relief to other pain medicines.
They work by reducing the chemicals in the body that produce ‘inflammation’ (inflammation produces swelling and pain). Unfortunately, in reducing inflammation, they also tend to temporarily reduce your immune system. We cannot control or counteract this. We cannot predict by how much, but research has indicated this can be by up to 50% reduction for 1 to 4 weeks. After this time it reverts to normal – it is not permanent.
There have been studies on influenza (flu) and pneumonia, and these have shown the risk of catching them is increased by steroid joint or soft-tissue injection. However, the increased risk is a small amount (under 1%). There is no known similar study that shows steroid injections to increase your chances of catching COVID-19 – but we suspect they can.
Further, we know the course of COVID-19 can be variable. In some people it is mild, in others it is severe or life-threatening. We know that severe COVID-19 infections are more common in older people and those who have other health problems. Cortico-steroid injections may increase the likelihood of severe COVID-19 infection if you catch it. In an attempt to reduce this risk, we sometimes do not perform cortico-steroid injections in higher-risk individuals. Your healthcare provider will discuss with you.
We also ask all patients to thoroughly try all other means of reducing their symptoms. We will discuss with you the alternative options you may or may not have tried or considered.
There are many complications from COVID-19, such as ‘vasculitis’ (inflammation of the blood vessels). This can be mild and temporary, giving you chilblains, or severe, such that you can develop gangrene in the foot. These issues can sometimes occur after you’ve had COVID-19 and you have recovered. We do not know the effect of cortico-steroid injections on these COVID-19 complications, but it is important you are aware of the issue.
We need to avoid inadvertently giving you a cortico-steroid injection if you have COVID-19. If you have the symptoms of temperature, cough or loss of taste/smell, either currently or in the last 14 days, you must inform us. After the injection you may be asked to maintain very strict social distancing and/or isolate for a specified period of days. This may impact on your work, family or social arrangements, but is unavoidable where advised.
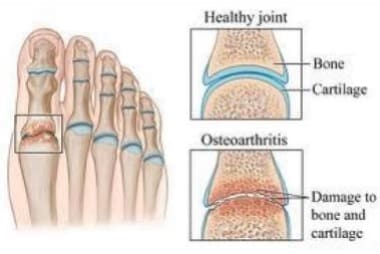
First Metatarsophalangeal joint (big toe) Osteoarthritis
What is it?
This is one of the most common types of foot osteoarthritis (wear and repair). It affects women and men, usually aged between 40-70 years of age. It can affect one foot, or both feet.
Features
- Joint enlargement
- Pain
- Bump on the top of the joint
- Stiffness
- Mild redness
- Can cause other parts of the foot to become painful through altered pressure.
What causes it?
- Age
- Trauma (stubbing the toe or it being trodden on)
- Tighter fitting shoes
- Family history
- Occupation and weight-bearing hobbies
- Bodyweight
- Foot shape and structure
- Tight leg muscles, weak arch muscles
What is the injury process?
The big toe is the largest of the toe joints and is the primary pivot point for our bodyweight when moving forward and your foot is pushing off the ground. The toe joint needs to flex but, at the same time, hold the weight of the body. It therefore carries very large forces over a small area and is susceptible to damage as a result.
Factors that can increase the damaging forces are things like impact, such as stubbing the toe, or if your foot is trodden on. Also, repetitive forces that are applied gradually over time can be a problem. These can be issues such as a longer toe bone, collapse of the foot arch and bodyweight. Shoes that are tight or high heeled can be issues.
How does treatment work?
The aim of treatment is to reduce pain. This is usually best achieved by lifting pressure off the joint and, in later stages, limiting how much it bends. The earlier you do this the better the outcomes will be.
How to manage it
Big toe osteoarthritis can be painful, or can also occur painlessly. If there is no pain, no treatment is required. Pain may not be there at all times and can vary from bad to non-existent.
Advice useful for all patients:
- Wearing wider, supportive footwear with a stiffer sole. Footwear needs to be flat, wide, with fastening and toe box to not irritate the top of the toe. Changing to this type of footwear is critical to relieving pain.
- Using insoles can reduce the pain – they may have a pad to take the weight off the joint and an arch support can also lift weight away from the joint. Sometimes using a stiff insole to stop the toe flexing can help.
- An insole inside the shoe should not make the shoe tighter, larger shoes may be needed. It is often worth spending time trying insoles with different designs to find one that works for you.
- Shoes and insoles will usually help about 50% of the time
- A toe spacer can help hold the toe straighter and relieve pain
- Exercises that deal with any muscle tightness or weaknesses may help: http://glos[1]care.healthandcarevideos.com/podiatry/49214 Research has found tight calf muscles will tend to mean you put more weight on the ball of the foot which is unhelpful, so stretching these is commonly recommended. Also, strengthening arch and leg muscles can help take some load off the toe joint
- Changing your work or hobbies to reduce prolonged standing. Hobbies that put lots of pressure on the toe – dancing, running, football.
- Reducing your weight to a normal ‘body mass index’ (BMI) by calorie-controlled diet. A normal BMI should be under 28 – https://www.nhs.uk/live-well/healthy-weight/bmi-calculator
- Use pain relief such as ibuprofen or paracetamol, unless you are not able to take these medicines – always consult your GP or Health professional.
Useful links
- https://www.nhs.uk/conditions/osteoarthritis/
- https://www.versusarthritis.org/about-arthritis/conditions/osteoarthritis/
Other pain management strategies
You can benefit from other pain management strategies such as:
- Mindfulness
- PACING
- Mental distraction
This can help you to self-manage or alternatively seek support from other health professions and groups.
Will I need further treatment?
The majority of people’s symptoms are managed using the simpler measures. This is acceptable, as these carry less risk. Further measures are usually only used when you are unable to cope with the pain and other treatments are not working. These are not used solely because the toe is very stiff or the joint is very large. Bear in mind, pain from osteoarthritis can be episodic and can change from severe back to mild/non-existent.
- The initial measures should be tried for 6-12 months. It is very important to ensure all the measures are in place before further treatment is considered.
- Usually at this stage X-rays and other investigations may be needed.
- Image-guided steroid injection. This is a potent dose of painkilling medicine – this can be done with an ultrasound or X-ray picture to improve accuracy and efficacy. This needs 48-hour rest and can feel worse initially. After settling, this can give benefit to many patients within 6 weeks, and for up to six months. It can be repeated up to three times. Risks include, but are not limited to, pain, making your pain worse, infection, scar tissue, bone necrosis and nerve injury.
Surgery
- Would only be considered in severe cases, and only after all measures have been tried, including trying variations of them more than once.
- There are some variations of surgery for toe joints and surgeons will need to evaluate you carefully to select the right approach.
- In some cases, they will cut open the foot from the side and they trim off prominent bumps and worn areas.
- In more advanced cases, they will put in screws to fix the joint together so there is no movement. The screws stay in permanently.
- You are still able to walk with a stiffened toe joint, but some other activities/sports may be more difficult.
- This will require three months recovery with 6 weeks of limited weight bearing.
- Risks – worsening of the pain, infection, painful scar tissue, non-healing bones, poor correction, nerve damage and chronic pain syndrome.
FAQs
- Should I stop exercise?
Activity is helpful. Using the joint doesn’t wear it out. Avoiding using it can stiffen it more. However, you may need to modify the type of activity you are doing. For example, ‘can I run?’ Yes – up a hill? Maybe not. Try to avoid modifying your walking due to fear of pain. - Can’t you put a lubricant in the joint to preserve it?
There are injectable medicines that in theory act as ‘lubricants’, such as hyaluronic acid. However, there is limited evidence as to their effectiveness with helping osteoarthritis. The National Institute of Clinical Excellence (NICE), whose guidelines we are governed by, does not recommend their use. Other ideas are being researched such as platelet-rich plasma and stem cell, but again, there is a lack of evidence for effectiveness. - Can I wear high heels?
You may be able to wear high heels for short periods. However, you may experience an episode of pain as a result. Constant use is to be avoided. - Will I get it in other parts of my body?
Big toe osteoarthritis is often caused by trauma to the big toe. It is less like hip osteoarthritis, which wears out through normal use. - Why can’t I have surgery straight away?
In Gloucestershire, eligibility for surgery on big toe joint osteoarthritis is based on strict criteria; part of which includes having to show you have complied with non-surgical measures. This is because simpler measures can be successful in many cases, and this helps you to avoid unwanted complications that can arise with more invasive measures. - Can I have a joint replacement?
This will be decided upon in your surgical consultation. However, a joint replacement is carried out less often, as it has a greater risk of complications and is not suitable for all.
Forefoot neuroma – 'Morton’s Neuroma'
What is it?
A common condition that can occur in the ball of the foot. It is a chronic irritation of a nerve inbetween the toe joints of the ball of the foot. The nerve enlarges after a period of time and forms a thickened lump called a neuroma. It affects women much more than men; typically aged between 40-70 years of age.
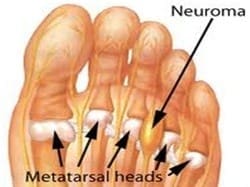
Features
The symptoms can be localised burning pain. It can radiate to the toes and also have a tingling nature. Usually there is no swelling or anything to see.
- Burning, numbness, tingling
- Sensation of scrunched-up socks underfoot, or something in the shoe
- Toes can become displaced
- Needing to take shoes off
- Commonly affect: third to fourth toes
- Less commonly affected: second to third toes.
What causes it?
There are factors associated:
- Tight-fitting footwear
- Foot shape and structure
- Tight leg muscles and weak arch muscles
- Body weight
- Occupation and weight-bearing hobbies
- Presence of a bunion and toe deformities
- Age
- Female
What is the injury process?
The damaged nerve is one of the nerves in the ball of your foot that gives you feeling. It is thought that the nerve gets damaged by being squeezed by tight, hard footwear or being overweight. Additionally, the nerve can be stretched by bending the toes excessively – e.g. wearing high-heeled shoes, or when your foot flattens, the change in your foot shape can cause the nerve to stretch and irritate. This squeezing and stretching causes the nerve to become thickened – this is the neuroma.
Typically the amount of damage accumulates slowly over time. Often you will not be aware of it happening earlier on, with the pain or altered sensation only presenting after this process has been occurring for a long time.
How does treatment work?
The key to making this better is to effectively reduce the squeezing and stretching though the ball of the foot. This is CRUCIAL and can be carried out in lots of ways that can be combined together.
The earlier you start managing the symptoms and comply with them, the better the outcomes will be.
How to manage it
- Footwear needs to be flat, wide, with fastening and deep, as not to irritate the tops of the toes. It should have a thick cushioned sole. Changing to this type of footwear is critical to recovery.
- A pain-relieving insole inside the shoe should not make the shoe tighter. It may have an offloading hole at the location of pain and a pad just behind the pain area to lift it up. When wearing it you should feel pressure is lifted off the painful area.
- Shoes and insoles will usually help about 50% of the time
- Re-lacing footwear to reduce tightness in the ball of the foot can help
- Exercises that deal with any muscle tightness or weaknesses may help – http://glos-care.healthandcarevideos.com/podiatry/49214
Research has shown that having tight calf muscles causes you to put more pressure on the ball of your foot. Tight calf muscles usually arrive from doing a sitting job and they tighten as we age. This is why calf stretching is recommended.
- Changing your work or hobbies to reduce prolonged standing
- Reducing your weight to a normal ‘body mass index’ (BMI) by calorie-controlled diet. Normal BMI should be under 28 – https://www.nhs.uk/live-well/healthy-weight/bmi-calculator/
- Using pain relief such as ibuprofen or paracetamol, unless you are not able to take this medicine – always consult your GP or health professional.
Do I need further treatment?
The majority of people’s symptoms are managed by implementing the simpler measures. This is acceptable, as this carries less risk. Further measures are usually only used when you are unable to cope with the pain and other treatments are not working. Bear in mind that pain can be episodic and can change from severe back to mild/ non-existent.
When the condition has been bothering you at least six months, further measures will be considered. Usually at this stage, imaging scans and other investigations may be considered. Neuromas can be present on a scan, but not be causing pain in up to 60% of the population. Scans therefore have the potential to be misleading. Further treatment will only be considered if the condition is painful enough.
- Ultrasound guided steroid injection: This is a potent dose of painkilling medicine to the nerve. To ensure accuracy and efficacy, this is best done with the aid of an ultrasound picture and it requires one appointment. It requires 48 hours rest and can temporarily feel worse. After this it often helps quickly. This treatment helps most people within one month and about 50% of people by six months. It has risks – pain, making the pain worse, infection, skin and soft tissue thinning and nerve injury. If successful it can be repeated with at least a six-month gap, up to a maximum of three to the same site.
Surgery
Research indicates larger neuromas in younger people proceed to surgery more often. A successful outcome seen in around 70% of people. This would only be considered after all measures have been tried, often trying variations of them more than once.
Surgery involves:
- This involves a cut into either the top or bottom of the ball of the foot. The nerve is cut away and removed.
- This will require three months recovery with six weeks of limited weight bearing.
- Risks – making pain worse, infection, painful scar tissue, painful regrowth of the nerve and chronic pain syndrome.
FAQs
- Can I wear high heels?
High heels are a key cause of neuroma development. You may be able to wear high heels for short periods. However, you may experience an episode of pain. Constant use is to be avoided. - Will normal feeling ever return to my toes?
This can depend on how long you have had the symptoms; the theory being the longer the nerve has been irritated, the more damaged it is and less likely to recover. It is common for there to be a degree of continued numbness and this is accepted as a good outcome. - There are other treatments available – why aren’t you offering those?
There are injectable medicines, such as hyaluronic acid. However, there is limited evidence in their effectiveness at helping neuroma.
Other surgical options include: cryotherapy (this is the process of freezing the nerve) and radiofrequency oblation (this is the process of burning the nerve). Therefore, the National Institute of Clinical Excellence (NICE), that we are governed by, does not recommend their use. Other ideas are being researched, such as stem cell injections, but again, there is lack of evidence for effectiveness.What we offer are the treatments that are backed by research and time tested. Neuroma are a common problem and prone to being longstanding and, as such, many new treatments are invented or offered. We are always reviewing our management strategies in line with the best evidence.
Hallux Valgus (bunion)
What is it?
Hallux valgus is the medical term for a bunion. It is the most common type of toe deformity and affects women much more than men. With a bunion, the big toe slowly becomes misaligned. It can occur on one or both feet and may or may not cause pain.
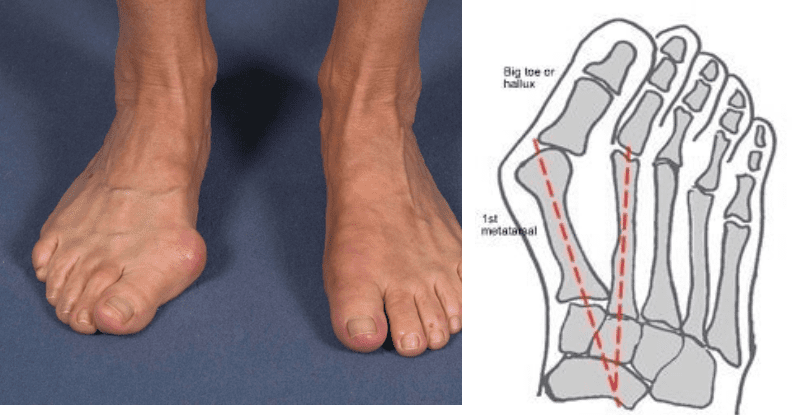
Features
- Big toe angles towards second toe
- Joint protrudes and becomes very prominent
- Redness over the bump
- Toes crowding
What causes it?
There are factors associated to this condition:
- Age
- Tighter-fitting shoes
- Family history
- Occupation and weight-bearing hobbies
- Bodyweight
- Foot shape and structure
- Tight leg muscles, weak arch muscles
What is the injury process?
The cause of bunions not entirely understood, but it is thought that in some individuals the joint is unstable, which leads to the altered position. People with flattened feet, or certain types of arthritis (e.g. rheumatoid arthritis), may develop a bunion (or bunions). The condition may be worsened by the wearing of tightly-fitting, narrow-toed shoes.
The big toe joint plays a key function in helping us move forward (propulsion). When a bunion develops, this stretches the surrounding soft tissues, which stops the joint from becoming straight again. As the position of the joint changes it is no longer able to tolerate the same pressure and function and becomes painful.
Typically a bunion occurs over a long time. In the early stages you may be aware of the bump forming, but pain may occur much later. You may also develop a bunion, but have no pain at all.
How does treatment work?
The aim is to slow the progression of the bunion and reduce pain from the change in foot shape by reducing pressure on the toes, so they don’t crowd each other, and on the bump itself, by wearing well-fitting shoes.
Insoles help address the function of the joint and alleviate pressure.
The earlier you start to manage the symptoms, the better the outcome will be.
How to manage the condition
- Footwear: Wearing wider, supportive footwear and using insoles can reduce pain. Shoes need to be flat, wide and deep, with fastenings, to avoid irritating the tops of the toes. Changing to this type of footwear is critical to relieving pain.
- A pain-relieving insole should not make the shoe tighter. It may have an offloading hole at the location of pain and a pad just behind the pain area to lift it. Arch support may help.
- Shoes and insoles will usually help about 50% of the time.
- A toe spacer can assist in holding the toe straighter and relieve pain.
- Exercises that deal with any muscle tightness or weaknesses may help – http://glos-care.healthandcarevideos.com/podiatry/49214
- Changing your work or hobbies to reduce prolonged standing
- Reducing your weight to a normal ‘body mass index’ (BMI) by calorie-controlled diet. Normal BMI should be under 28 – https://www.nhs.uk/live-well/healthy-weight/bmi-calculator/
- Using pain relief, such as ibuprofen or paracetamol, unless you are not able to take these medications. Always consult your GP or healthcare professional.
- The toe can only be straightened with surgery. However, you may not need this if the deformity is small, or the pain is manageable.
Will I need further treatment?
If there is no pain, no treatment is required. Simpler measures should be tried for 6-12 months. It is very important to ensure those are in place before trying others. Usually at this stage X-rays and other investigations may be needed.
Ultrasound guided steroid injection: This is a potent dose of painkilling medicine – generally this is not used for the treatment of bunion pain.
Surgery
Severe cases may be operated on, for example:
- the deformity will not fit any footwear
- the pain is very bad most of the time
- the toe position is causing other toe issues
- the bunion is stopping you from performing your job or other daily necessary functions.
There are many variations of surgery for bunions and a surgeon will need to evaluate you carefully to select the right approach. In most cases the surgeon will open the foot from the side and make carefully-angled incisions in the foot bones, to reposition them into alignment.
The surgeon will trim prominent bumps and insert screws to hold the bones in alignment. The screws stay in permanently.
Recovery will take at least 3 months, with 6 weeks of limited weight bearing
Risks include, making pain worse, infection, painful scar tissue, non-healing bones, poor correction, nerve damage and chronic pain syndrome. This would only be considered after all measures have been tried, often trying variations of them more than once.
Please note, surgery will not be performed for cosmetic reasons alone.
FAQs
I don’t like the look of my bunion and I’m limited with shoes I can wear – why can’t I have surgery?
Eligibility for surgery in Gloucestershire is based on strict criteria. These include having to demonstrate you have complied with non-surgical measures. This is because simpler measures can be successful in many cases, and avoid the unwanted complications which might arise from more invasive measures.
Surgery carries many risks and benefits. However, the risks have to be justified. Typically this is performed in scenarios of non-improvement, pain and/or significant functional loss. Sometimes after surgery appliances and supportive footwear still need to be worn.
Hallux Valgus (bunion) surgery
What is offered?
Hallux valgus, or ‘bunions’, may or may not cause pain. If there is no pain, no treatment is required. Mild pain and smaller deformity is managed without surgery.
Surgery is carried out to straighten the toe and reduce the prominence, effectively narrowing the foot. If you have other toe deformities that are painful, these will usually be dealt with at the same time. If you have two feet that need surgery, this may be done simultaneously or one after the other. This is a decision made in conjunction with the surgical team.
What does surgery involve?
- You may have either a general or local anaesthetic
- When you are asleep, or the foot is numb, the surgeon will cut into the skin to get to the foot bones – avoiding nerves and blood vessels
- They will use an electrical bone saw to make precise cuts
- The cut bones are moved into a better-aligned position
- The bones are fixed in place with screws and the screws stay in permanently
- Stitches are then used to close the incision.
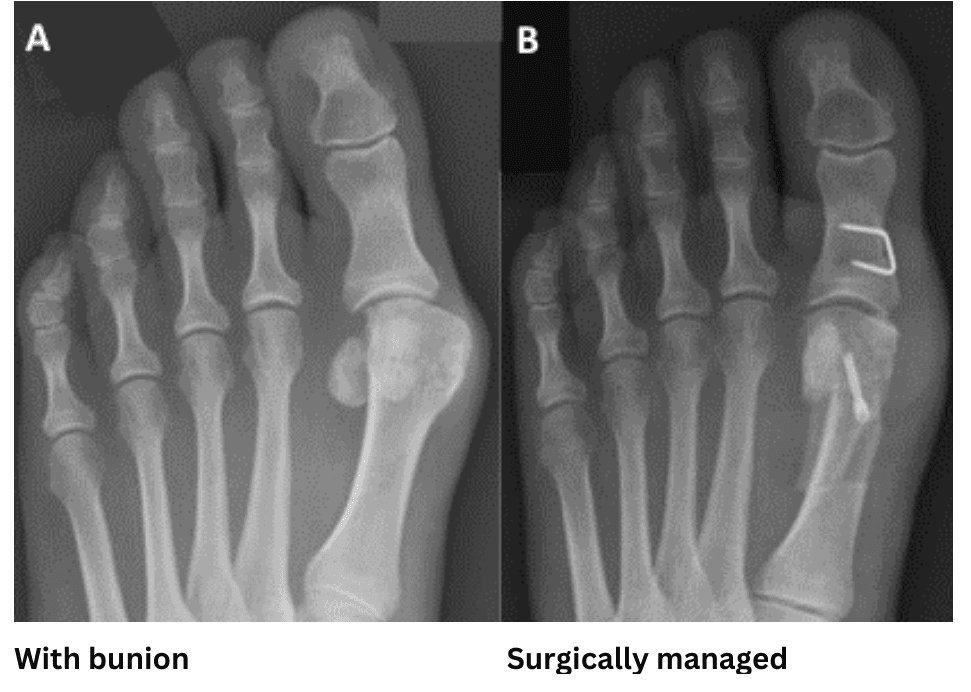
After surgery
- You may be in plaster and non-weight bearing for 6 weeks. This is to give the bones chance to heal
- Pain relief may be required and may be given to you by your surgery team or GP
- Stiches will be removed at 4-6 weeks
- At around 6 weeks you will go back into flat, roomy shoes – e.g. sports shoes
- You will be given exercises to mobilise and strengthen the toe.
- Swelling and tenderness can persist for a long time and full recovery can take up to 12 months.
Risks
- Pain: This may be temporary post-operative pain; also sometimes for a long time after. Very rarely pain can be permanent.
- Infection can sometimes happen and will need to be treated with antibiotics or other measures
- Infrequently the metal screws may cause irritation. If this happens they may need to be removed.
- The bones usually heal well, but sometimes they don’t and may need further surgery
- Nerves can get damaged during surgery or healing
- Very rarely a form of chronic nerve pain, called chronic regional pain syndrome, can develop – and this can be permanent.
FAQs
- Will my bunion come back?
There is reasonable chance of a small bunion recurrence. However, this is often non-painful and manageable. Very occasionally, a second toe correction surgery will be required.
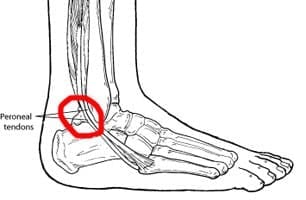
Peroneal tendon pain
What is it?
Tendons are pieces of connective tissue which join muscles to bones. The peroneals are a group of two muscles on the outside (little toe side) of the leg, and they have tendons that join them to the side of the foot.
When they are damaged, we often experience a pain that develops behind the ankle bone, or where the tendon is attached on the outside of the foot. It affects women and men equally.
Features
- Pain
- Swelling around the tendon
- Loss of power
- A feeling of instability
What causes it?
There are factors associated to it:
- Trauma
- Occupation and weight-bearing hobbies
- Foot shape and structure
- High arch
- Ankle sprain
- Bodyweight
- Tight leg muscles
- Some neurological conditions
What is the injury process?
It is thought the peroneal tendons become damaged by being overstretched or placed under pressure. The tendons pass around the ankle, through a lining known as the peroneal sheath.
Their function is to point the foot down and turn it way from the body .Often problems arise when they are needed to perform this function too often – such as when your foot naturally leans outwards. The tension can increase to a level that damages the tendon.
Typically the amount of damage accumulates slowly over time. Often you will not be aware of it happening earlier on with the pain only presenting after this process has been occurring for a long time.
There are different grades of tendon injury:
- Tenosynovitis: Inflammation of the sheath – this is the early stage of the injury process
- Tendinopathy: Wear and tear of the tendon. This is usually seen with some thickening of the tendon tissue and weakening. This is a more chronic injury which may be accompanied by sheath inflammation.
- Tendon tear: This is most often a split in the middle of the tendon secondary to the tendinopathy getting worse. This can very occasionally develop into a full rupture. Often a small amount of wear and tear on the tendon can be a normal part of the aging process and is picked up on ankle scans without any symptoms. In these cases often no treatment is required. Tears can also occur painlessly in around 40% of the population. Tears should only be addressed/treated if they are painful.
X-ray may also indicate the presence of accessory bone. This is a normal variant where there is an extra piece of bone next to the tendon in the side of the foot. Most of the time this is irrelevant, however, it can cause irritation to the tendon as it glides over or be irritated itself.

How does treatment work?
Your treatment may differ depending on the stage your foot presents with. The aim is to reduce pain and reduce worsening deformity. This is achieved by effectively reducing the load through stretched soft tissues and attempting to improve strength in the foot and ankle. This is CRUCIAL and can be done in lots of ways that can be combined together.
An insole that tilts the foot inwards helps reduce the load through the tendons when walking
A brace can give greater stability and support and may be considered in advancing cases
The earlier you start managing the symptoms, the better the outcome.
How to manage peroneal tendon pain
Peroneal tendon pain is usually diagnosed in the early stages with a simple examination – X-rays and scans are not always needed.
With early intervention the majority of patients can be treated successfully without surgery by:
- Wearing supportive footwear/boot
- Avoiding walking barefoot and/or wearing unstable footwear – shoes that are too flexible, high heels, shoes that are very worn down at the heel.
- Changing your occupation or hobbies to reduce prolonged standing
- Using insoles that reduce the pain – this is typically an insole that is built up on the outside (little toe side), avoiding insoles that have lots of arch support
- A pain-relieving insole should not make the shoe tighter – larger shoes may be needed. It is often worth spending time trying different insole or ankle support designs to find one that works.
- Shoes and insoles will usually help about 75% of the time
- An ankle brace can be used to further reduce movement
- Ankle braces and foot insoles can be either readymade or custom. It is worth trying the readymade first as this is quicker.
- Reducing your weight to a normal ‘body mass index’ (BMI) by calorie-controlled diet normal. BMI should be under 28 – https://www.nhs.uk/live-well/healthy-weight/bmi-calculator/
- Exercises that deal with any muscle tightness or weaknesses may help: http://glos-care.healthandcarevideos.com/podiatry/49214 We usually recommend calf stretches and building up the outside leg muscles – the peroneals.
Research shows tight calf muscles cause increased load to the ankle. Tight calf muscles usually result from performing a sitting job and they tighten as we age. This is why calf stretching is recommended.
We also recommend strengthening of the soft tissues on the outside of the ankle to make them better and supporting.
Using pain relief, such as ibuprofen or paracetamol, is suggested – unless you are not able to take these medicines. Please consult with your GP or healthcare provider.
Will I need further treatment?
Following the above measures will usually see peroneal tendon pain ease in around 6-12 months. It is very important to ensure all these are in place before moving on to further measures.
- If the condition has been bothering you for at least six months, further measures will be considered. Imaging scans and other investigations may be considered.
- Ultrasound guided injection: This is a potent dose of painkilling medicine. This is only used if there is a significant degree of swelling around the tendon (sheath). To ensure accuracy and efficacy this is best done with the aid of an ultrasound picture and requires one appointment. You should rest for 48 hours after this procedure. This treatment helps most people within one month and about 50% of people by six months. It has risks – pain/worsening, tear of tendon, infection, skin and soft tissue thinning, and nerve injury. Rupture rate is low but can happen.
- Aircast boots and casts: These can be used to significantly reduce the load on the ankle for a period of time – usually 6-12 weeks. This can give it rest to help it settle. Risks include pain/worsening, soft tissue weakening, calf blood clots (deep vein thrombosis).
- A stronger brace can be worn in your normal footwear to help support the ankle when walking. This can be custom made (Richie brace).
Surgery
- This is rarely required and usually when the tendon is significantly torn. Surgery may be reserved only for those who are in pain and active.
- Surgery involves cutting away unhealthy areas of the tendon and repairing tears and splits. Sometimes another tendon is used to repair them. You may be in plaster – healing time is around three months.
- If the tendon injury is not improving due to a structural issue, e.g. very high arch foot, changing the foot shape may be considered. This means cutting the heel bone and sliding the lower part of the heel outwards. This is a bigger procedure with a long recovery period (six months).
- Accessory bones are rarely surgically managed, but can be removed if having a considerable impact on the tendons.
FAQs
- Will I have to wear the shoes/insoles/brace all the time?
The more you wear them, the more improved your symptoms are likely to be. Realistically, they need to be worn at least 80% of the time. - It hurts a LOT, is this normal?
A peroneal tendon injury can be very painful and potentially incapacitating. Following an exercise-based rehabilitation plan and using some form of support (insoles, ankle brace), where appropriate, is the most effective way of reducing pain and restoring function. Pain avoidance and fear of movement are common. Speak to a healthcare professional for advice on how to protect and strengthen the ankle. - Will I need a scan?
A scan is not always required – a peroneal tendon injury can be diagnosed by a physical examination. Often, management of peroneal tendon pain will be the same with or without the scan. If your symptoms are not improving after a reasonable period of time, a scan may be considered. - Wouldn’t this be resolved more quickly with surgery?
No tendon injury resolves quickly. Surgery carries risks and tendons need a lengthy surgical recovery.
Soft tissue and joint injections
How will I benefit from a steroid Injection?
- To reduce the pain and swelling to the inflamed joint or structure
- To break down or reduce the formation of scar tissue.
What are the alternatives?
All treatment options for your condition should have been discussed by your clinician. These may include medication, physiotherapy, exercise, insoles or changes of footwear.
When might a steroid injection not be right for you?
- If you feel unwell or have any form of infection
- If you have any known allergy to steroids or local anaesthetic
- If you have diabetes
- If you have a joint replacement at the site of injection
- If you have any recent trauma at the site of injection
- If you have had recent surgery or surgery planned
- If you have problems with liver or kidneys
- If you are on medication to suppress your immune system
- If you are on medication to thin your blood
- If you have had a vaccination in the last 2 weeks
- If you have had a steroid injection to the same site previously.
What are the possible side effects?
As with any medical procedure there are always risks involved. The following responses are rare but can occur:
- Infection
- Allergic reaction
- Soft tissue atrophy (local pitting of the skin, more likely with repeated injections)
- Tendon rupture
- Skin changes – the skin at the site may become whiter and dimpled – this may resolve with time
- Post-injection flare – a temporary increase in pain for 3-4 days. This will settle with rest and painkillers
- Blood sugar elevation – if you have diabetes you may notice this. It should return to normal in 7-10 days
- Facial flushing – reddening of the cheeks, usually settles in 24-48 hours.
If you notice any of these side effects you must notify your clinician or GP.
What happens on the day of the injection?
- You will be assessed by the injecting clinician to ensure a steroid injection is right for you. You may be asked about your medical status.
- You will asked to consent and given an opportunity to discuss the benefits and risks of a steroid injection before it is carried out
- You may be given a local anaesthetic to numb the area – this will leave it numb for 2-6 hours
- It may be advisable to have someone drive you
- We recommend you rest the day and the following day.
What happens after the injection?
A steroid injection can take time to have an effect. When the anaesthetic wears off the area is likely to be as painful as before, or even a little worse. To help with this we recommend the following:
- Take your preferred painkiller – commonly this will be paracetamol or ibuprofen. However, do not use these if you are already taking painkillers prescribed for you by your GP
- Use an ice pack. Place the pack, wrapped in a damp tea towel, over the area for 10 minutes. This can be repeated every hour.
- To give the steroid injection the best chance of being effective in the long term, you must listen to the advice given by your clinician; especially regarding modifying your activities, performing exercises, changing your footwear and using any supports you may have been given.
How quickly does it work?
The steroid may start to work over a 2-3 day period, but can take 4-6 weeks for full effect.
How many injections can I have?
This depends on the area being injected. Generally injections are not repeated in the same area within three months of each other.
How will I be followed up?
This will be discussed at your injection appointment.
Vascular disease
Vascular disease is the collective term for diseases of the veins and arteries. Every part of the body to which blood flows can be affected by it. It’s as common as cancer and heart disease, and accounts for 40% of deaths in the UK, many of which are preventable.
Useful links
Podiatry Clinic Locations
Bourton
George Moore Community Clinic, Moore Road, Bourton on the Water, GL54 2AZ
Dursley
Vale Community Hospital, Dursley, GL11 4BA
Stroud
Stroud Theapy Centre, Level 4, 1 King Street, Stroud, GL5 3BS
Newent
Holts Health Centre, Watery Lane, Newent, GL18 1BA
Lydney
The Health Centre, Albert Street, Lydney, GL15 5NQ
Moreton-in-Marsh
North Cotswolds Hospital, Stow Road, Moreton-in-Marsh, GL56 0DS
Cheltenham
St Paul’s Medical Centre, 121 Swindon Road, Cheltenham, GL50 4BW
Cinderford
The Health Centre, Dockem Road, Cinderford, GL14 2AN
Fairford
Fairford Hospital, The Croft, Fairford, GL7 4BB
Southgate Moorings
Kimbrose Way, Gloucester, GL1 2DB
Coleford
The Health Centre, Railway Drive, Coleford, GL16 8RH
Churchdown
Albermarle Road, Churchdown, GL3 2HE
Stonehouse
The Health Centre, The Car Park, High Street, GL10 2NG
Cheltenham Independent Living Centre
Village Road, Cheltenham, GL51 0BY
Cirencester
Cirencester Hospital, The Querns, Cirencester, GL7 1UY
Gloucestershire Royal Hospital
Great Western Road, Gloucester, GL1 3NN
Winchcombe
Winchcombe Medical Centre, Greet Road, GL54 5GZ
Cheltenham General Hospital
Sandford Road, Cheltenham, GL53 7AN
Tewkesbury
Tewkesbury Community Hospital, Barton Road, Tewkesbury, GL20 5GJ


