Allied Health Professionals
Allied Health Professionals are the third largest clinical workforce in the NHS. Made up of 14 unique and diverse professions, their practice is integral to most clinical pathways.
What is an Allied Health Professional?
Allied Health Professionals (AHPs) work across organisational boundaries, providing solution-focused, goal-centred care to support patients’ independence.
We have 10 of the 14 Allied Health professions working within our Trust.
Art Therapists
Art therapists use art as a form of psychotherapy to encourage clients to explore a variety of issues including emotional, behavioural or mental health problems, learning or physical disabilities, life-limiting conditions, neurological conditions or physical illnesses.
To find out more about Art Therapy/Psychotherapy, click here
Meet Fiona Williams, Trust Lead for Arts Therapies
Drama Therapists
Drama therapy is a form of psychotherapy. Drama Therapists are both clinicians and artists that draw on their knowledge of theatre and therapy to use as a medium for psychological therapy that may include drama, story-making, music, movement and art.
Patients and service users are able to explore a wide variety of different issues and needs, from autism and dementia to mental illness in an indirect way, leading to psychological, emotional and social changes.
Drama therapists work with their clients using a very wide range of dramatic techniques in verbal and non-verbal ways. Though vocalisation, story-making and talk are integral parts of drama therapy, the practice does not necessarily rely on spoken language alone to resolve what a patient may wish to address, explore or to seek support with.
Kim Diment, Drama Therapist
Drama Therapist Kim is part of the Dementia Education Team at Charlton Lane Hospital. She has been working clinically on the acute assessment ward with dementia patients for several years, but feels very privileged to be able to go onto the ward once a week wearing her AHP hat.
She enjoys trying to make a connection with people who may be non-verbal and no longer able to express their emotions and feelings. Through movement, music, sensory work, narrative, stories and poems, Kim tries to find that common humanity we all share, and that is why she’s so proud to be an AHP.
Podiatrists
Podiatrists are part of the team of Allied Health Professionals that specialise in the foot, ankle and leg, leading the patient through the whole journey including prevention, diagnosis and treatment.
What’s a podiatrist?
Dietitians
Dietitians work as integral members of multidisciplinary teams to treat complex clinical conditions such as diabetes, food allergy and intolerance, IBS syndrome, eating disorders, malnutrition, frailty, kidney failure, coronary heart disease, dysphagia and neurological disorders.
They advise and influence food and health policy across the Trust, and support catering and nursing colleagues to ensure that any food provided for service users in our settings is to a high standard which meets national hospital food standards and is specifically tailored to the nutritional needs of the patients. This means separate menu cycles for our community hospitals, learning disability settings, eating disorders day treatment unit and mental health inpatient sites.
Some examples of where you will find us:
Marie, Head of Profession for Dietetics
Marie joined us last year from our Specialist Community Diabetes Team and brings with her a strong background both in clinical and leadership experience in her roles prior to joining the Trust.
Marie joined the Community Diabetes Specialist Team in Gloucestershire in December 2019 and has been instrumental in ensuring people have continued to receive the dietetic advice and support they need throughout the pandemic, providing phone and remote consultations when face-to-face clinics ceased to run.
Jennifer, Specialist Dietitian
Jennifer works as the Specialist Dietitian for inpatients in the Trust’s seven community hospitals. Her role includes supporting individual patients, staff training, development of policies and ensuring high-quality service and patient-centred care. Many of the patients she works with are older adults with complex co-morbidities and her role includes supporting patients on the stroke unit with enteral nutrition following PEG insertion.
Dan, Eating Disorders Clinician
In his Care Home Support role, Dan provides education to care home staff, empowering them with the knowledge to provide better nutrition and hydration care to their residents, while also acting as a point of contact for care homes when they have nutrition and hydration concerns about specific residents.
Jo, Macmillan Specialist Community Dietitian
Jo’s current role is with the Macmillan Next Steps Rehabilitation team, promoting healthier lifestyle choices for those affected by breast, colorectal, prostate and haematological cancer in Gloucestershire. Many people experience eating concerns either before, during and/or after their treatment for cancer. Some of these concerns may include unintentional weight loss or weight gain, cancer-related fatigue, gastrointestinal problems following surgery or radiotherapy and swallowing difficulties. Dietitians play a key role in supporting people living with and beyond cancer by assessing and managing the effects of cancer treatment and reducing the risk of malnutrition or secondary cancers (and other conditions like diabetes, cardiovascular disease etc.) through appropriate nutritional counselling and support.
Sarah, Specialist Diabetes and Cardiac Rehab Dietitian
In 2012 the opportunity arose to set up the dietetic service within the community diabetes team, and Sarah has been there ever since, leading on patient education for the county and managing a varied case load. The team delivers structured education for all people diagnosed with Type 2 Diabetes and sees patients on a one-to-one basis, helping them to gain control of their condition through lifestyle modification and appropriate treatment.
Sarah is passionate about ensuring equitable education and information is provided across the county, with informed patient choice being at the forefront of their care.
Jessica, Eating Disorders Clinician
Jessica is part of a specialist team which provides eating disorders day treatment. Based at the Brownhill Centre in Cheltenham, she supports patients with meal planning, nutrition education, weight restoration, and ensures the meals provided on site are suitable to allow patients to effectively negotiate the nutritional and psychological challenges that an eating disorder presents.
Occupational Therapists
Occupational Therapists (OTs) are experts in occupations and occupational science – this means the activities that we all complete in our daily lives, ranging from specific tasks such as self-care, to those life roles that we all have.
OTs work with their patients to look at how they approach these activities and to identify the barriers preventing them from completing these tasks or roles. Taking into account both their physical and mental health, they support them to be able to do the everyday activities they need or want to do to live a healthy and fulfilling life.
We have OTs working in both adult and children’s services across all our settings, not to mention our brilliant occupational therapy support staff, which includes OT Assistants and Technicians, Therapy Assistants and Therapy Practitioners.
To help demonstrate the wide range of activities and support our occupational therapists provide across the Trust, some of our fantastic OTs have produced these videos in which they speak about their roles and what they love about their jobs.
Wayne: Engagement Activity and Physical Health Practitioner
Click on the links below to view the films
- Tom: OT, Gloucester Recovery Service
- Olly: Assertive Outreach Team, Gloucester and the Forest of Dean
- Michelle: OT, Perinatal Mental Health Service
- Lucy: OT, Psychiatric Intensive Care Unit
- Gemma: OT Technician, Mental Health Services
- Laura: Occupational Therapy Student
- Angela: OT, Gloucester Recovery Service
Children’s Occupational Therapists
The Children’s OT service is an integrated countywide specialist service working at health, social services and educational sites across Gloucestershire. It aims to address the needs of children/young people who have difficulties managing their activities of daily living and developing functional skills such as bathing, showering, toileting, dressing, eating; we call these Occupational Performance Issues (OPIs).
Read more about the service here>
Adult Occupational Therapists
Working within our Integrated Community Teams (ICTs), our occupational therapists treat adults aged 18 years and over with physical and social problems, to improve everyday functions and support them to live independently and safely in their own homes.
This may range from adapting household products so that people can use them, to teaching different coping strategies, or helping people participate in social activities. Occupational therapists are problem solvers who empower people to take control of their lives.
Read more about the service here>
Learning Disability OTs
Learning Disability Occupational Therapists are present within the Community Learning Disabilities Teams (CLDTs) , the Learning Disability Intensive Support Service (LDISS) and Berkeley House.
Read more about the CLDT service here>
Specialist Palliative Care OT Service
The Specialist Palliative Care OT team works in partnership with patients to enable them to be as comfortable and productive as possible at end of life. They support people in living independently with a sense of control by maximising their functional independence and quality of life as much as possible. They work with patients to help them decide on the goals of their treatment, and tailor it to what is important to them.
Physiotherapists
Physiotherapy is a healthcare profession that works with people to identify and maximise their ability to move and function. Functional movement is a key part of what it means to be healthy.
This means that physiotherapy plays a key role in enabling people to improve their health, wellbeing and quality of life.
Adult MSK physiotherapy
Musculoskeletal Physiotherapy (MSK) is the assessment and treatment of patients with problems relating to the muscular system, joints and various other structures of the body. These structures might be affected by injury, pain, surgery, posture and dysfunction. The aim of the physiotherapist is to restore movement and function to the patient as efficiently as possible.
Read more about the adult physiotherapy service here>
Children’s physiotherapy
To find out more about the Children’s Physiotherapy Service, click here>
Musculoskeletal Advanced Practitioner Service
MSKAPS (Musculoskeletal Advanced Practitioner Service) is a specialist service which GPs and other healthcare professionals can refer to for assessment of a musculoskeletal problem (a problem with a person’s muscles, bones or joints, such as lower back pain) which has not been helped by the usual management methods for the condition, such as exercises, medication, rest, physiotherapy or podiatry. Click here to find out more>
Films: Why I’m Proud to be a Physiotherapist
Speech and Language Therapists
Speech and language therapists (SLTs) provide life-improving treatment, support and care for children and adults who have difficulties with communication, eating, drinking or swallowing.
SLTs assess and treat speech, language and communication problems in people of all ages to help them communicate better. They also assess, treat and develop personalised plans to support people who have eating and swallowing problems.
Using specialist skills, SLTs work directly with clients and their carers and provide them with tailored support. They also work closely with teachers and other health professionals, such as doctors, nurses, other allied health professionals and psychologists, to develop individual treatment programmes.
SLT services in Gloucestershire
All SLTs are registered with the Health and Care Professions Council (HCPC) and are members of the Royal College of Speech and Language Therapists (RCSLT). The HCPC and RCSLT have codes of practice, conduct and standards which govern SLT practice. There are three services provided covering Gloucestershire countywide: learning disability/mental health , adults and children.
Learning disability
The SLT clinicians are based within the Community Learning Disability Teams (CLDTs) and Later Life Services.
Eligibility
We support any adult who needs help with their communication and/or eating and drinking, and who has a diagnosis of a learning disability, is registered with a Gloucestershire GP, or funded by Gloucestershire CCG. We also support their transition from children’s to adult services.
We work with family members of people with a learning disability, GPs, hospitals, social workers and colleges, as well as other people who may need advice on how best to support someone with a learning disability.
We are part of a multidisciplinary team (MDT), which also includes occupational therapists, physiotherapists, psychiatrists, psychologists and nurses.
Adult Service (acute and community)
The service is split into the following specialist areas:
- Head and neck: Oncological and surgical cancer patients seen throughout treatment pathway. Laryngectomy service.
- Brain Injury: Acute, early discharge and community service for patients with a new ABI and rehabilitation needs.
- Voice: Community service for patients with neurological, organic, psychogenic and functional voice disorders. There is a service for transgender patients.
- Stroke: Based on the Hyper Acute Stroke Unit (HASU) at GRH and Stroke Rehabilitation Ward at CGH. Close links with the stroke service based at The Vale Community Hospital and Early Discharge Service.
- Community/out-patient: Covering ieight community hospitals / locations – The Dilke, Lydney, Cheltenham, Stroud, Tewkesbury, Cirencester, North Cotswolds, Southgate Moorings. Patients are seen in clinic or for home visits. A Parkinson’s Group is run regularly.
- Augmentative Alternative Communication (AAC): Offering assessment, advice and trials of low and high-tech aids.
- General inpatients (GRH and CGH): Patients are referred from across wards (e.g. respiratory, care of the elderly, intensive care) for swallowing and communication needs.
Also provided are voice and instrumental swallow clinics: Videofluoroscopy (VFS) and Fiberoptic Endoscopic Evaluation of Swallowing (FEES).
Children’s Service
The Children’s Speech and Language Therapy countywide service provides assessment, diagnosis, advice and intervention for children and young people aged 0-18 years where there is a concern regarding:
- Language delay
- Developmental language disorder
- Phonological/speech delay and disorder
- Social communication difficulties
- Hearing impairment
- Swallowing difficulties
- Elective and selective mutism for primary school-aged children
- Voice problems
- Cleft lip and palate
- Stammering
- Augmentative alternative communications (AAC)
Parents and education staff are recognised as key partners and we aim to empower them to support the development of their children’s communication skills. This includes providing appropriate information, support and training to enable other professionals to identify developmental needs and deliver therapeutic interventions and some elements of specialist programmes guided by the speech and language therapist.
Further information about the Adult Speech and Language Therapy Service can be found here>
Further information about the Children’s Speech and Language Therapy Service can be found here>
Films: Why I’m Proud to be a Speech and Language Therapist
Speech and Language Therapist Linda is a very proud AHP. She qualified in 1993 and now works primarily with secondary school-age students who are not in education for one reason or another. Linda finds her role fascinating, rewarding, interesting, stimulating and thought-provoking – and can’t understand why everybody doesn’t want to be a speech and language therapist!
In this short film members of the Speech and Language Therapy team at Cheltenham General Hospital explain why they are all so proud to be Allied Health Professionals.
In this short film, members of the Speech and Language Therapy team share the many and varied reasons why they are proud to be Allied Health Professionals and what they love most about being AHPs.
Emma is a Speech and Language Therapist who works with children and young people who stammer. She is proud to be an AHP because her profession is all about giving children and young people the confidence and skills they need to make their voices heard.
Speech and language therapist Gemma works in the Autism Diagnostic Assessment Service. She is proud to work in a great multidisciplinary team and to be able to give answers and information to people who have been struggling with their communication and interaction for the majority of their lives.
Osteopaths
Osteopaths take a holistic view of the structure and function of the body to diagnose and treat a wide variety of medical conditions.
Their work is centered on the principle that the skeleton, muscles, ligaments and connective tissues of an individual need to function smoothly together so as to maintain wellbeing.
Osteopaths use a number of non-invasive treatments such as touch, physical manipulation, stretching and massage to restore bodily equilibrium through increasing the mobility of joints, relieving muscle tension, enhancing blood and nerve supply to tissues, and encouraging an individual’s own healing mechanisms.
Osteopaths use physical manipulation, stretching and massage with the aim of:
- increasing the mobility of joints
- relieving muscle tension
- reducing pain
- enhancing the blood supply to tissues
- helping the body to heal
- They use a range of techniques, but not medicines or surgery.
When it’s used
Most people who see an osteopath do so for help with conditions that affect the muscles, bones and joints, such as:
- lower back pain
- uncomplicated neck pain (as opposed to neck pain after an injury such as whiplash)
- shoulder pain and elbow pain (for example, tennis elbow)
- arthritis
- problems with the pelvis, hips and legs
- sports injuries
- muscle and joint pain associated with driving, work or pregnancy
To find out more visit the NHS website>
Paramedics
In recent years the paramedic profession has evolved from being a provider of emergency treatment and transportation in an ambulance to a provider of mobile healthcare.
When not responding to emergencies, Community Paramedics can help people manage chronic diseases such as diabetes, high blood pressure, cholesterol and prevent disease and illness through immunisations and screenings. They can provide information and counselling about ways to care for themselves and their families.
Paramedics can now be found working in multiple settings, including general practice, minor injury units, urgent care centres, walk-in centres and accident and emergency (A&E) departments, telehealth and telecare services and in remote and offshore sectors.
Paramedics in some of these settings often undertake advanced clinical assessments and take the responsibility for the ongoing care provided to patients, in addition to onward referral and discharge.
Operating Department Practitioner (ODP)
An Operating Department Practitioner (ODP) is a vital part of the operating theatre team.
An ODP provides individualised and skilled care for patients at all stages of their operation – from when they arrive in the operating theatre department, to discharge from the recovery room.
An ODP works across three main areas within the operating theatre – anaesthetics, surgery and recovery – and is responsible for preparing the environment and all of the necessary instruments and equipment in readiness for an anaesthetic, surgery or recovery of patients.
Hello, my name is…
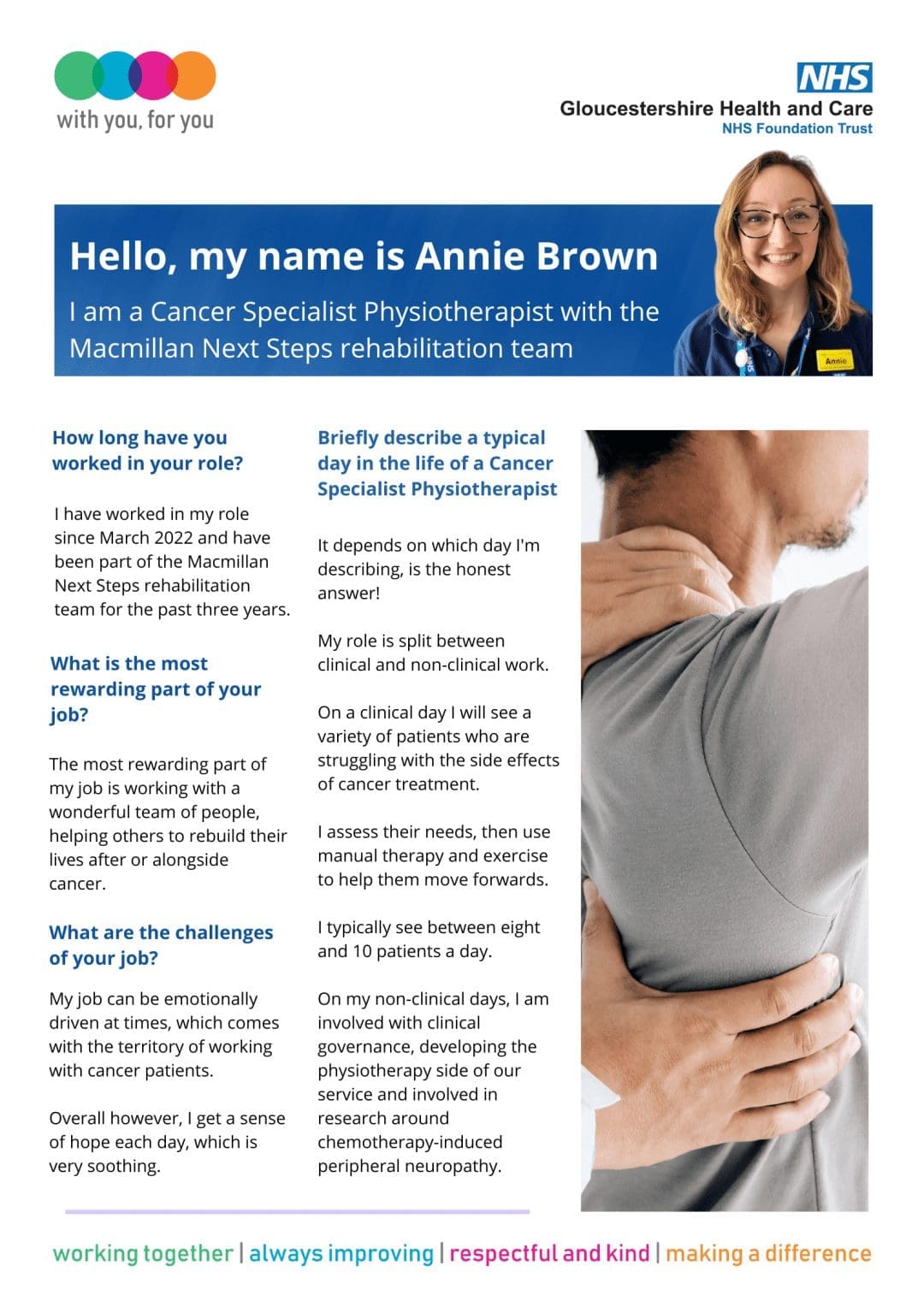
Annie Brown
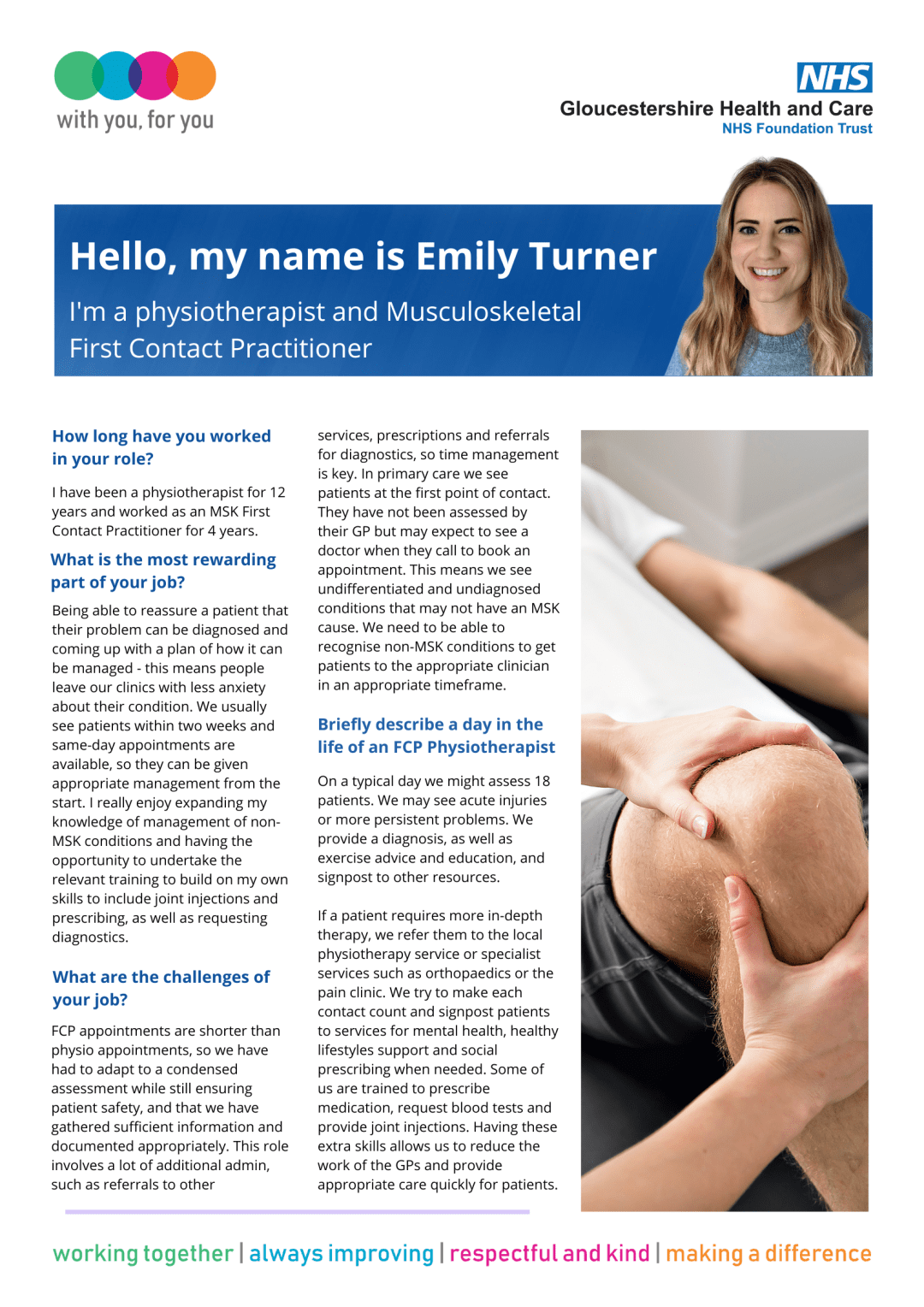
Emily Turner
Louise Thorpe

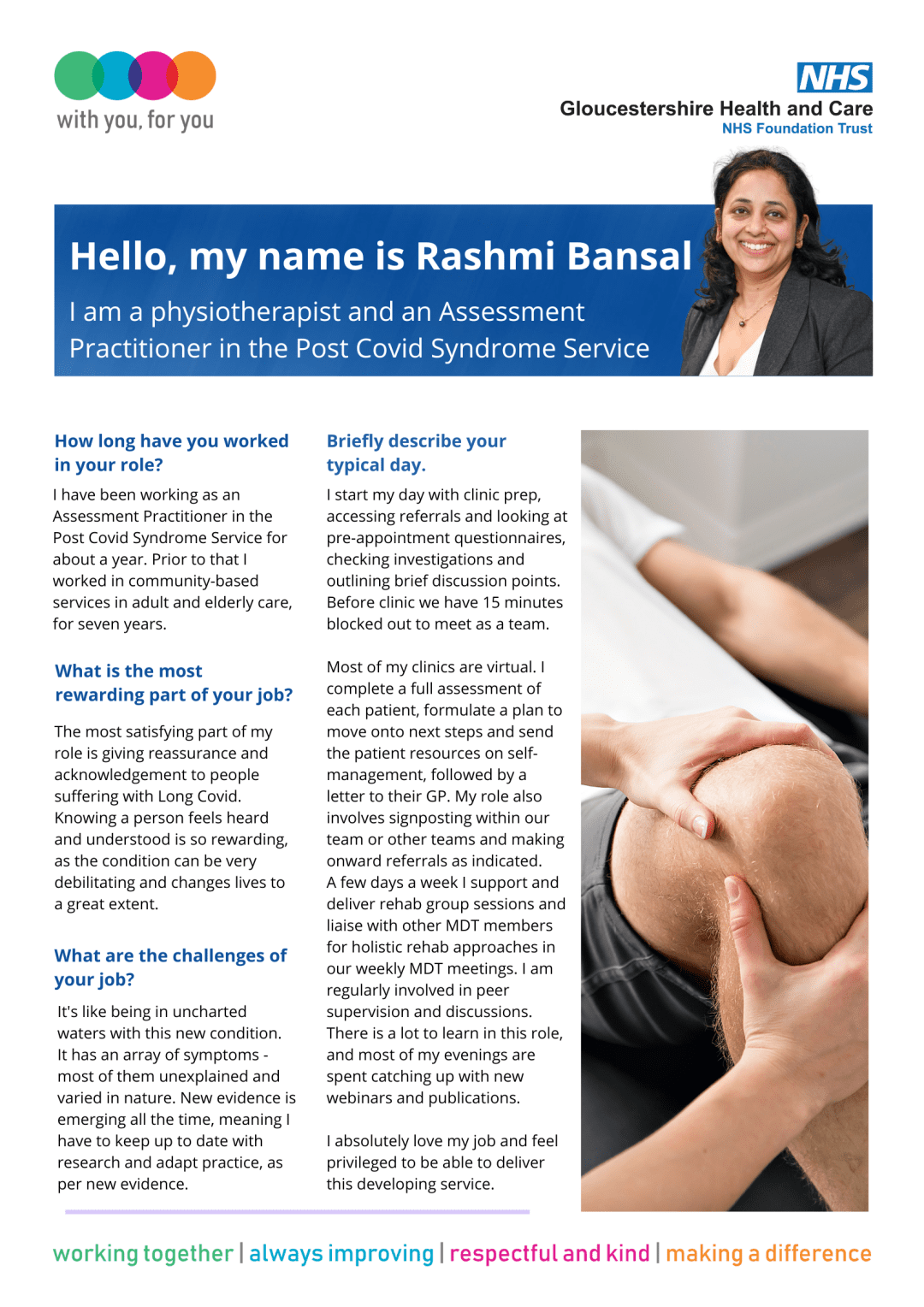
Rashmi Bansal
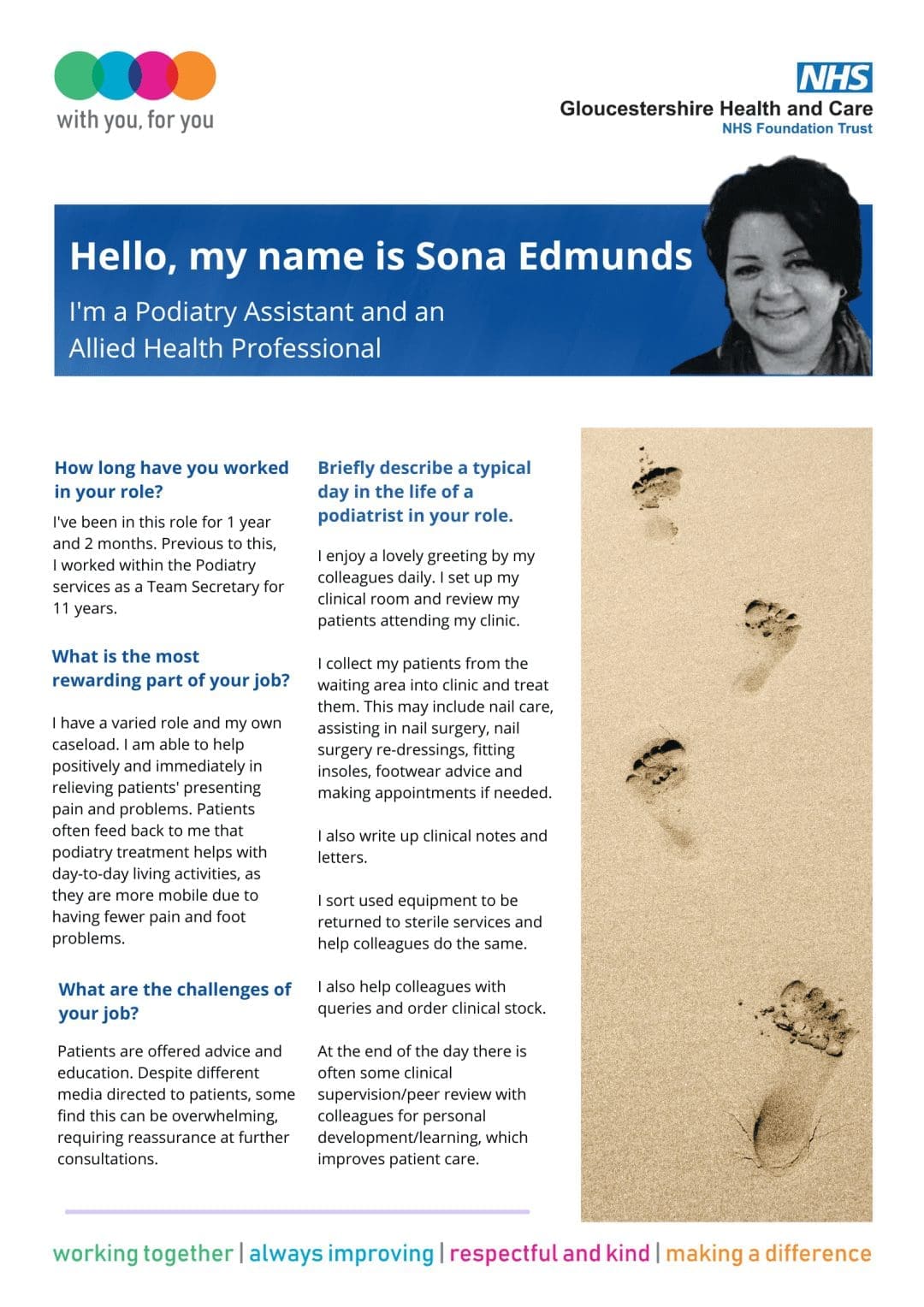
Sona Edmunds
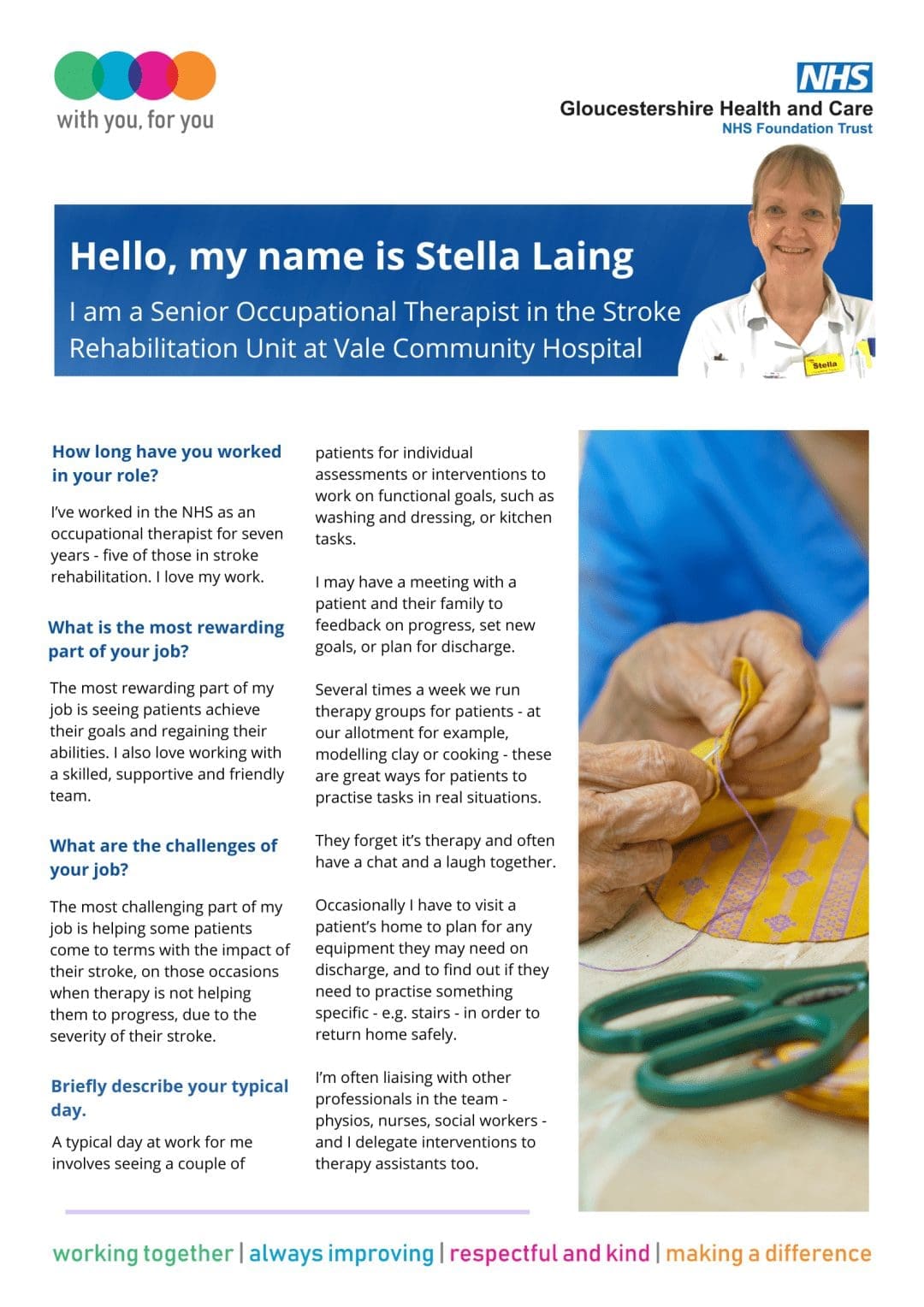
Stella Laing

AHP Support Workforce Education and Career Development Programme
Health Education England has established this national Allied Health Professions (AHP) support workforce programme to help us recognise, develop and expand our non-registered AHP workforce.
We’re proud of the role our AHP support workers play in providing high-quality, life-changing care for our patients and service users across services in Gloucestershire. But we know that historically across the country, there has been variation in their education and training and how they are deployed.
This is why we’ve committed to developing consistent, occupation-specific and sustainable education and career development pathways for all our AHP support workers by April 2024.
About the programme
We are working to ensure that:
- Our patients and service users have access to skilled and consistently well-trained support workers who have a defined role within their team
- Our AHP support workers have access to development structures that provide opportunities to follow a richer and more rewarding career pathway
- Our services can address the current variation in support worker roles, banding and progression
- Our support worker roles can be at the heart of improvements in service delivery and transformation, including new models of care.
Find out more about the Gloucestershire AHP Support Workforce Programme here>
Resources
HEE has published a suite of resources to help us prepare for the implementation of its Allied Health Profession (AHP) Support Worker Competency, Education and Career Development Framework.
The Readiness Toolkit provides a step-by-step approach to implementing the Framework, utilising quality improvement approached and helpful links.
Click here for the full range of resources.
Contact us
If you’d like to find out more or to get involved in the programme, contact our AHP Support Workforce Programme Lead Kerrie Hodges: kerrie.hodges@ghc.nhs.uk

