News & Views
Read the latest news from Gloucestershire Health and Care NHS Foundation Trust

Farewell Celebration for Trust Chair, Ingrid
Colleagues, former colleagues, partners, volunteers, Experts by Experience and family members...
Dementia Action Week – May 13-19
Colleagues will be out and about across Gloucestershire in May helping people to understand how to...

Using Cognitive Behavioural Therapy to Manage Stress
Not feeling like yourself right now? Maybe you’re feeling irritable, worried, scared, struggling...

A new community hospital for the Forest of Dean
Gloucestershire Health and Care NHS Foundation Trust is working on a new community hospital in the...

Community Mental Health Transformation Newsletter – March 2024
Since we shared our last update in January, there has been further progress on the Community...

Grants Totalling £300k For Projects to Support Mental Health
The Community Mental Health Transformation (CMHT) programme, led by Gloucestershire Health and...

Twiddle mitts bring a splash of colour to Windrush Ward
Patients and colleagues at Cirencester Hospital were thrilled and very grateful to receive these fabulous twiddle mitts from talented knitter Margaret in Bradley Stoke, Bristol.

Countryfile star opens ‘fantastic’ new cabin and workshop
Our therapeutic allotment at Montpellier received a special visit on Friday from farmer and BBC TV presenter Adam Henson, who dropped in to officially open the site’s newly-constructed cabin and workshop.

A look back at Nutrition and Hydration Week 2024
Last week was Nutrition and Hydration Week (11-17 March) – an annual campaign which focuses on the links between our health and what we eat and drink.

New Chair Selected for Trust
A new Chair has been selected for Gloucestershire Health and Care NHS Foundation Trust. Graham...

Today is International Long COVID Awareness Day
Today (15 March) is International Long COVID Awareness Day. Now in its second year, the campaign aims to raise awareness of the symptoms of Long COVID, and the NHS support available to those suffering from the condition.

Gloucestershire Health and Wellbeing College Summer Courses
Our Gloucestershire Health and Wellbeing College team has released details of their summer courses...

Celebrating Tewkesbury CATU Anniversary
Our Community Assessment and Treatment Unit (CATU) held a Tea Party on Monday (11 March) to mark...
It’s Nutrition and Hydration Week!
This week (11-17 March) is Nutrition and Hydration Week – an annual event with a shared, global objective to reinforce, focus, energise and create activity and engagement to promote nutrition and hydration as a fundamental element to maintaining health and wellbeing within health and social care.

Positive workplace picture from Staff Survey results
Our Trust's Staff Survey results were released yesterday, reflecting the positive outlook of...

Better Care Together Awards – The Winners!
More than 135 colleagues gathered to celebrate our Better Care Together awards at Hatherley Manor...

Immunisation service to continue delivery of national programme
Our School Age Immunisation Service (SAIS) is delighted to be continuing delivery of the national school-based immunisation programme in Gloucestershire.

Campaign launched to drive up childhood vaccinations
The UK Health Security Agency (UKHSA) has today launched a campaign across England to remind parents and carers of the importance of making sure their children are vaccinated against serious diseases – some of which, such as measles and whooping cough, are re-emerging in the UK.

Physiotherapy in the Forest: Helping local residents to regain their confidence
GHC Musculoskeletal (MSK) Physiotherapists Tomas Bullock and Cerys Watcyns are based in the Forest...

State-of-the-art cataract microscope at Tewkesbury Hospital
The countywide Ophthalmology Cataract Service is provided in partnership by Gloucestershire...

Speech and Language Therapy training
Our Speech and Language Therapy department is running two training courses designed to help...

Marking five years of The Vale Stroke Unit
Our Specialist Stroke Rehabilitation Unit team has been joined by commissioners, League of...

Use of Meta Pixel on our website
It has been brought to our attention that the Trust, along with a number of other NHS and other...

A look back at National Apprenticeship Week 2024
Last week was National Apprenticeship Week 2024. The Apprenticeship and Widening Participation team hosted a packed programme of events throughout the week reflecting this year’s theme, Skills for Life.

Community blood pressure and health checks
Our Community Outreach Vaccination and Health team, together our One Gloucestershire health...

Mental Health Courses to Restart
Gloucestershire Talking Therapies is restarting face-to-face courses. The courses are aimed at...

National HIV Testing Week 2024
It’s National HIV Testing Week (5-11 February). Every year this annual campaign, run by HIV Prevention England, aims to raise awareness about the importance of regular testing, to help reduce the number of people living with undiagnosed HIV and those diagnosed late. The number of people diagnosed with HIV is falling, but there is still work to do.

It’s National Apprenticeship Week!
It’s National Apprenticeship Week (5-11 February). The theme for #NAW2024 is Skills for Life, which reflects on how apprenticeships can help individuals develop the skills and knowledge they need for a rewarding career, and how employers can develop a talented workforce equipped with future-ready skills.

New Film Encourages Health Checks
A new film has been produced to encourage people with serious mental illnesses (SMI) to access...

Measles: Parents urged to ensure their children are protected
With the number of reported measles cases in young people in the UK on the rise, the School Age Immunisation Team at Gloucestershire Health and Care NHS Foundation Trust is urging parents and guardians of children in Years 8 to 11 (aged 12 to 16) to check their MMR status and make sure they are fully vaccinated against the disease.

It’s not too late to get your Covid booster!
If you’re living in Gloucestershire and haven’t yet taken up the opportunity of a Covid booster, our Outreach Vaccination and Health team and local pharmacies are offering drop-in vaccination clinics to those who are eligible.

Not Been Feeling Like Yourself Lately?
According to recent research, nearly half* of those living in the South West felt concerned about...

Farm visitors bring a ‘Good Day’ to Charlton Lane Hospital
Last week, Charlton Lane Hospital in Cheltenham received a special visit from residents of The Good Day Farm in Chipping Campden – a mobile farm which brings its animals to the community.

Community Mental Health Grants – Second Opportunity to Apply
A new round of grants are being made available to Voluntary, Community and Social Enterprise...

Blood pressure: Know your Numbers
The NHS in Gloucestershire is urging people aged 40 and over to get 2024 off to a healthy start by dropping in at a community location for a blood pressure check.
NHS expands mental health support for veterans
The NHS is rolling out an expanded mental health support service for Armed Forces veterans, as a...

Community Mental Health Transformation Newsletter – Edition 5
Since we shared our last update in September, there has been further progress on the Community...

Industrial Action – Changes to Services in Gloucestershire
Members of the British Medical Association - Junior Doctors - will take industrial action from...

Seven New Queen’s Nurses for Trust
Colleagues from our Trust have been given the prestigious title of Queen’s Nurse (QN) by community...

Cosmo and Nigel bring festive cheer to community hospitals
This week colleagues and patients at two of Gloucestershire’s community hospitals have welcomed a pair of special visitors from Cotswold Vale Alpacas.
Cosmo and Nigel embarked on tours of the wards at North Cotswolds Hospital in Moreton-in-Marsh on Monday (11 December) and Tewkesbury Community Hospital yesterday (Thursday 14 December).

Ward Sister Lou wins award for dementia tool
Congratulations to Ward Sister Lucinda (Lou) Williams on scooping the ‘Seeing Me Award’ at this year’s South West Integrated Personalised Care Awards. Lou, who specialises in dementia care, was celebrating with her colleagues on Abbey View Ward at Tewkesbury Community Hospital this morning, after picking up the award at last night’s glittering ceremony at Darlington Hall in Totnes, Devon.

Occupational Therapist Neil Scoops National Award
Congratulations to Occupational Therapist Neil Withnell, who was crowned Housing Occupational...

Sign up as an NHS Cadet
NHS Cadets is a programme created by St John Ambulance in partnership with the NHS. It’s designed...

Festive Friends and Family event at Montpellier Unit
Montpellier Low Secure Unit in Gloucester hosted another successful friends and family event last Friday (8 December). This was an opportunity for service users to welcome their friends and family, introduce them to members of the multidisciplinary team and for everyone to enjoy a festive-themed buffet – all of which was planned, shopped for and prepared by the residents on Montpellier.

World AIDS Day – 1st December
Friday 1 December is #WorldAIDSDay – a global campaign by the National AIDS Trust, which has been recognised on 1st December every year since 1988. Its aim is to support those living with HIV, remember those who have lost their lives to AIDS-related illness, secure the rights of people living with the condition and continue the fight to end the stigma surrounding HIV.

Children’s flu – it’s not too late to vaccinate!
With Flu season now well underway, our School Aged Immunisation Team would like to take this opportunity to remind parents of the importance of protecting their children against the virus by ensuring they have their flu vaccination.

Trust presented with Defence ERS Gold Award
Representatives from Gloucestershire Health and Care NHS Foundation Trust were extremely proud and honoured this morning to receive the Defence Employer Recognition Scheme (ERS) Gold Award from the Wessex Reserve Forces’ and Cadets’ Association (WRFCA), in recognition of its commitment and support for defence personnel.
16 Days of Action campaign – 25 November to 10 December
The 16 Days of Action campaign commences Saturday 25 November, International Day for the...

New clinic rooms for mental health team
Colleagues in Cheltenham's mental health services celebrated on Wednesday (Nov 15) to mark the...

Survey: Reducing inequalities in Sexual Health (RiiSH 2023)
Surveillance data concerning sexually transmitted infections (STIs) has shown large increases in bacterial STI diagnoses among gay, bisexual and other men who have sex with men (GBMSM) attending sexual health services (SHS) in England between 2021 and 2022.

Charlton Lane Hospital enjoys a flying visit!
Charlton Lane Hospital in Cheltenham recently enjoyed a flying visit from Gerald, Henry and Wally...

World Diabetes Day: Know Your Risk!
Today is #WorldDiabetesDay. Around 200,000 people are diagnosed with type 2 diabetes every year, and you don’t need to be one of them.
Finding out your risk of type 2 diabetes only takes a few minutes – it could be the most important thing you do today. Find out your risk here: https://riskscore.diabetes.org.uk/start
Our Community Diabetes Team supports people with type 2 diabetes in managing their condition to the best of their ability. People may be referred to the service for a variety of reasons.

Colleagues lay wreath as part of Poppies to Paddington initiative
To mark Remembrance Day (11 November), Great Western Railway organised its annual Poppies to...

Better Care Together Awards – Nominate Now
We will be holding an awards ceremony on 7 March 2024 to celebrate the outstanding commitment,...

Plaque Unveiled in Honour of District Nursing Founder
Professional Head of Community Nursing, Nancy Farr, was invited to unveil a plaque in honour of...
Council of Governors – Nominations Open Now
Nominations are now open for you to join our Council of Governors. Our Council needs the following...

Occupational Therapy Week 2023
This year’s Occupational Therapy Week starts today (Monday 6 November) and finishes on Sunday 12 November. As a profession, Occupational Therapists are on the frontline of health equity and are uniquely placed to understand and tackle the challenges people face. OTs see health inequalities every day, supporting and helping those most in need.
Introducing the Patient and Carer Race Equality Framework (PCREF)
We are working with NHS England to implement the first ever anti-racism framework for mental health Trusts and service providers. The Patient and Carer Race Equality Framework (PCREF) will ensure that we are responsible for co-producing and implementing concrete actions to reduce racial inequality within our services, with a view to becoming an actively anti-racist organisation.

Cavell Award for Tewkesbury Ward Sister Lou Williams
Our Tewkesbury Ward Sister Lou Williams has been presented with a prestigious Cavell Star Award...

Trust hosts its first ever AHP Community of Practice Forum
Our Trust held its first ever AHP Community of Practice Forum yesterday (Monday 16 October)...

Recruitment Underway for New Chair
Recruitment is underway to find a new Chair for Gloucestershire Health and Care NHS Foundation...
Recruitment for New Director of Nursing, Therapies and Quality
Following the recent announcement that our Director of Nursing, Therapies and Quality John...

Forest of Dean Hospital Update
The new Forest of Dean Community Hospital is due to open in Spring 2024 and we have recently...

Pastoral Care Quality Award for Trust
We’re delighted to have received the NHS Pastoral Care Quality Award for the high level of care...

Patient Safety Award Commendation
A trust project received a high commendation in the annual Health Service Journal Patient Safety...

Gloucestershire Health & Wellbeing College courses – 2023
Our Gloucestershire Health & Wellbeing College (formerly the Recovery College and Glos Self...

Falls Awareness Week 2023
Join our Falls Education Services at events across the county, starting on Monday 18 September,...

HPV vaccination programme moves to single dose
The Human papillomavirus (HPV) vaccine helps to prevent HPV-related cancers from developing in boys and girls. While most types of HPV are harmless, some high-risk types can lead to the development of cancers, including cervical cancer, cancers of the head and neck (mouth and throat) and cancers of the anus and genital areas.

Sexual Health Week: 11-17 September
Today marks the start of Sexual Health Week. Being safe means feeling empowered to access contraception, testing and treatment. It means understanding consent, healthy relationships and pleasure. It also means providing relationships and sex education (RSE) that gives young people the tools to navigate the world safely – both online and offline – and delivering safe, accessible sexual health services, wherever people need them. That’s why for #SHW23 we’re #PlayingItSafe!

Community Mental Health Transformation: Small Grants
As part of the national programme of Community Mental Health Transformation, we are introducing a...

Mental Health Act Managers
We're looking for a number of Mental Health Act Managers, who have a unique and very important...

Parents urged to protect their children against flu
As we enter the 2023-2024 flu season, the Immunisation Team at Gloucestershire Health and Care NHS...

Supporting those in need of emergency mental health support in Gloucestershire
You may have heard of a new initiative called Right Care, Right Person, which may change the way...

DIALOG training for VCSE Organisations
Training is being offered to people working in voluntary, community and social enterprise (VCSE)...

Falls Prevention Awareness Week: September 18-22
Gloucestershire Health and Care NHS Foundation Trust is committed to empowering all older adults in Gloucestershire to reduce their risk of falls, which are one of the greatest causes of serious injuries and death among people over age 65. On September 18-22, GHC is partnering with the National Council on Aging (NCOA) to mark Falls Prevention Awareness Week.

Community project shortlisted for HSJ award
A joint NHS community project in Gloucestershire to tackle health inequalities has been...

New Mental Health Training Dates
Free training is being offered to voluntary, community and social enterprise (VCSE) partners...

Veterans Moving Forwards recovery course
The autumn programme of recovery course Veterans Moving Forwards starts next month. The course has been co-produced with veterans and is offered by Gloucestershire Health and Wellbeing College.

Industrial Action Update
Changes are being made to local NHS services as a result of industrial action by Junior Doctor...

Community Mental Health Survey 2023
We believe providing high quality mental health care for everyone is fundamentally important....
Results Day Support for Students
Our Apprenticeships and Widening Access Team are offering support for those getting their results...

School-based vaccination catch-up clinics
Our immunisation team is offering ‘catch-up’ clinics for children who have missed their...
World Breastfeeding Week: 1-7 August
World Breastfeeding Week officially kicks off tomorrow, each year celebrated around the world from 1-7 August. Gloucestershire Health and Care NHS Foundation Trust’s Health Visiting team offers a range of support, including advice on positioning, attachment, hand expressing and assisting you and your family to continue to breastfeed for as long as planned. If problems occur, your health visitor can refer you to our Specialist Breast Feeding team.

Hope House sexual health community clinics reopen
Hope House is pleased to announce its face-to-face community clinics are up and running again. Due to Covid-19 our clinics at Coleford Health Centre, Stroud, Cirencester and Tewkesbury community hospitals, Hartpury University, Hartpury College and the Royal Agricultural College, have been restricted to telephone and video consultations only.

New sensory room at Evergreen House officially opened
A new sensory room has been opened at Evergreen House in Cheltenham, thanks to the generosity of a local children’s charity.

‘My Life’ unveiled at GL1
NHS colleagues and individuals with lived experience from Gloucester gathered at GL1 last week to...

New display name format for emails – from 1 September
From Friday 1 September, the way the names of GHC colleagues is displayed in Outlook and MS Teams...

International Self-Care Day – 24 July 2023
The World Health Organisation's Self-care Month ends Monday 24 July with International Self-Care...

Community Nurses Medical Bags
Community Nurses are feeling the benefit after the Trust invested in new medical bags to organise...

Community Mental Health Transformation Newsletter – Edition 4
Since we shared our last update in May, we've made even more progress on the Community Mental...

Quality Mark for Preceptorship Programme
We are proud to announce that we have been awarded the National Preceptorship Interim Quality Mark...

BMA Junior Doctors’ industrial action – Thursday 13 July (7am) to Tuesday 18 July (7am)
BMA Junior Doctors’ industrial action – Thursday 13 July (7am) to Tuesday 18 July (7am)....
Trust Support for Veterans Achieves Gold Award
We are proud to have achieved the Gold Employer Recognition Scheme Award for our work to support...
Public Governor Elections – Nominations Open Now
Nominations are now open for six Public Governor positions in the following areas: Public:...

Community Mental Health Survey
Our trust will soon be carrying out a survey, supported by the Care Quality Commission, to...

Trust named Large Employer of the Year in the SW Apprenticeship Awards
Gloucestershire Health and Care (GHC) is celebrating the news that it has been named Large...

A look back at National Healthcare Estates and Facilities Day
Today is National Healthcare Estates and Facilities Day – a time to recognise and celebrate the critical work of all E&F staff and their role in the provision of our healthcare services.

Last chance to get your spring Covid booster
Throughout Spring 2023 our Outreach Vaccination team has been offering boosters to those at highest risk of severe illness from Covid-19. The vaccine offers added protection if Covid rates are high over the summer months and reduces people’s chances of needing hospital treatment if they do catch the virus.

Trusts join forces to take on military challenge
Gloucestershire Health and Care joined forces with members of Great Western Hospitals NHS Trust to field a team in Exercise Medical Endeavour (formerly the South West NHS Military Challenge), which took place at Okehampton Army Training Camp over the weekend (16-18 June).

Cervical Screening Awareness Week: 19-24 June
This week (19-24) June is Cervical Screening Awareness Week – a campaign launched in 2021 to encourage those eligible for screening to respond to their cervical screening invitation letters and book an appointment at their GP practice or sexual health clinic if they missed their last one.

Allotment team celebrates national awards success
The Montpellier Allotment Project Team celebrated success at the national Design in Mental Health Community Awards when they received a ‘Highly Commended’ in the Outside Space of the Year category.

Mental Health Awareness Training
Free training is being offered to voluntary, community and social enterprise (VCSE) partners...

South West Apprenticeship Awards – we’ve made the finals!
We’re delighted to learn that Gloucestershire Health and Care is a finalist in this year’s South West Apprenticeship Awards

‘What Matters to You?’ Day – 6 June
Do you feel that the people you talk to in health or social care really understand what is...

Carers Week: 5-11 June 2023
Carers Week is an annual campaign to raise awareness of caring, highlight the challenges unpaid...

Community Mental Health Transformation Newsletter – Edition 3
It's Mental Health Awareness Week so the perfect time for us to share another update on Community...

Mental Health Engagement Events
Booking is now open for a series of engagement events to learn more about Community Mental Health...
Dealing with Anxiety
Mike Dexter is a Senior Psychological Wellbeing Practitioner with NHS Talking Therapies,...

Community Mental Health – Survey 2023
Our trust will soon be carrying out a survey to understand what you think about your care. This is...

Heart Failure Awareness Week 2023
Heart Failure Awareness Week, held every year in May, is an opportunity for us to shine a light on heart failure and to raise awareness about our fantastic Heart Failure Service at GHC. Led by the British Society for Heart Failure (BSH), the campaign aims to raise awareness of the importance of recognising heart failure symptoms early, getting an accurate diagnosis and receiving optimal treatment.

CAMHS text messaging
As part of our work to reduce missed appointments and ensure that only those who need our service...

Bank Holiday and Industrial Action
Cheltenham A&E to temporarily close from Friday 28 April (8pm) to Tuesday 2 May (8am)....

New home for NHS Gloucestershire Talking Therapies service
Our talking therapies service (formerly known as Let’s Talk) is moving into St Paul’s Medical Centre in Cheltenham.

Surprise retirement celebration for CEO Paul
Colleagues past and present gathered at Churchdown Community Centre yesterday (Thursday 30 March) to throw a surprise farewell celebration for our Trust’s CEO Paul Roberts, who is set to retire in April.

Better Care Together Awards 2023
Our Better Care Together awards took place this afternoon (23 March) at Kingsholm Stadium, in...

Community Mental Health Transformation Newsletter – Edition 2
There's been a lot happening since we sent our last newsletter out in January. This includes a...

CaSA – Charlton Lane’s new carers support group
CaSA (Care and Support Always) is a new monthly support group for carers of patients of Charlton Lane Hospital (whether current or recently discharged).
Trust celebrates 2022 Staff Survey results
Our Trust is delighted with its positive and encouraging results from the NHS Staff Survey...

Allotment team offer battery hens a new home – and lease on life!
Members of the Montpellier Allotment Project Working Party embarked on an...

Return to Practice: is it time to think about returning to the profession you love?
We're calling on Allied Health Professionals and Healthcare Scientists to return to the profession...

High Sheriff takes in progress on new Forest Hospital
The High Sherriff of Gloucestershire and Vice Lord Lieutenant of Gloucestershire were the latest...

New Associate Non-Executive Director for Board
A new Associate Non-Executive Director has been appointed to the Trust’s Board. Vicci...

Congratulations to our 2023 Apprenticeship Awards winners!
In celebration of National Apprenticeship Week (6-12 February), the Apprenticeship and Widening...
Community Mental Health Transformation Newsletter – edition 1
Community Mental Health Transformation (CMHT) is underway in Gloucestershire, with the Forest of...

King Street move for Physio and Podiatry
Stroud’s Podiatry and Adult Physiotherapy services have moved into the new £6.5m medical centre...

Teens could be missing out on potentially life-saving vaccinations
Parents and carers of Year 8 and 9 secondary school-aged children are being urged to take...

BBC Points West broadcasts live from Cirencester Hospital
With so much in the news about the pressures on acute hospitals, ambulance crews and GP surgeries,...

Royal Visit to Newly Developed Therapeutic Allotment
Her Royal Highness The Princess Royal visited our newly developed therapeutic allotment in...

Veteran Support Boosted by Step into Health
The support we give to serving military personnel, veterans and military families is set to be...

Our Carers’ Charter
Our Carers’ Charter was developed with, and for, carers as a joint statement of how we will work...

Visiting over the Christmas period
We know how important it is to our patients who aren’t able to get home just yet for loved ones to...

MIIU Closures – 20 December 2022
Members of the Royal College of Nursing are taking industrial action on 20 December 2022. Due to...

Industrial Action – 20 December 2022
NHS leaders in Gloucestershire have today provided advice to the public ahead of two days of...

Special hospital visitors Pringle and Widget spread a little festive cheer!
Penguins Pringle and Widget have been delighting staff and patients at two of our community...

Industrial Action: 15 December 2022
Members of the Royal College of Nursing are taking industrial action today (15 December 2022). Due...

Industrial Action – 15 December 2022
In response to the planned industrial action announced by the Royal College of Nursing (RCN), the...

New young people’s participation groups
We're inviting young people across the county to work with us to improve our services. We're...

Better Care Together Awards
Better Care Together awards launched to celebrate colleagues from Gloucestershire Health and Care NHS Foundation Trust.

Arts Psychotherapies
'Arts Psychotherapies' is an umbrella term for the four professions working psychologically and...

New Chief Executive for Trust
A new Chief Executive Officer has been appointed to Gloucestershire Health and Care NHS Foundation...

Celebrating Psychological Professions Week – 14-18 November
We're celebrating Psychological Professions Week and this year, the PPN national conference has a...

Oliver McGowan Mandatory Training launches in England
The long-awaited rollout of the Oliver McGowan Mandatory Training in Learning Disability and...

Sustainability
The Trust's Sustainability Strategy has just been published, laying out our approach for the next...

World Occupational Therapy Day
World OT Day was first launched on 27 October 2010 by the World Federation of Occupational Therapists (WFOT). Since then it has become an important date in the occupational therapy calendar to promote and celebrate the profession internationally.

Montpellier allotment redevelopment project
For years the Montpellier allotment and green space at Horton Road, Gloucester, has provided an...

Lord-Lieutenant presents Trust with Defence ERS Silver Award
Lord-Lieutenant of Gloucestershire, Mr Edward Gillespie OBE DL, presents veteran and GHC's Lead...
Access scheme for aspiring clinical psychologists from under-represented backgrounds
As part of our ongoing commitment to addressing issues of diversity and inclusion within the...

Public Sector Excellence Award for Trust
We've been crowned winners of the Public Sector Excellence category at the SoGlos Gloucestershire...
First and second COVID vaccines for children aged 5-17
It isn’t too late for children aged five to 17 to access a COVID vaccination if they haven’t...

Ceremony marks official reopening of Stroud’s Jubilee Ward and MIIU
NHS colleagues and Stroud Hospital League of Friends jointly celebrated the official reopening of...

Looking After Number One – World Mental Health Day 2022
Looking after number one, this World Mental Health Day.

Baby Loss Awareness Week, 9-15 October 2022
Our Perinatal Mental Health Team is supporting Baby Loss Awareness Week - a week for bereaved...

Ward refurbishment work underway at Cirencester Hospital
Work to improve the patient experience as well as fire safety on the wards at Cirencester Hospital has recently started. Our Trust is upgrading the fire compartmentalisation on both Windrush and Coln Wards…

Apprenticeship Award Success for GHC
Gloucestershire Health and Care NHS Foundation Trust was named Employer of the Year for the second...

Bank Holiday Monday: information on local health services
The NHS in Gloucestershire joins the rest of the country in sending our deepest sympathies to the...
Community Mental Health Transformation in Gloucestershire
The NHS Long Term Plan and NHS Mental Health Implementation Plan 2019/20 – 2023/24 set out that...

CQC Congratulates Trust on ‘Very Good’ Report
The NHS Trust providing community physical, mental health and learning disability services for...
Monkeypox: Halting the spread
Since the first case of monkeypox was reported in the UK earlier this year, we have seen an...

Annual General Meeting – Come Along!
Our Annual General Meeting is taking place on Tuesday 20 September, from 5.30 to 6.45pm. The event...

Stroud Hospital refurbishment completed
Following an extensive £2m building project Gloucestershire Health and Care NHS Foundation Trust...

Stroud MIIU to close for three days in preparation for return to hospital
Stroud Minor Injuries and Illness Unit (MIIU) will close for three days starting on Tuesday 2...

NHS rainbow badges and lanyards
NHS rainbow badges and lanyards You may have spotted some of our staff wearing NHS rainbow badges...

New Anti-Social Behaviour Pledge for Gloucestershire
A pledge has been signed by Gloucestershire leaders, promising that anti-social behaviour will be taken seriously, made easier to report and tackled in partnership.

New Non-Executive Director Appointed to Trust Board
A new Non-Executive Director called Nicola de Longh has been appointed to the Board of Gloucestershire Health and Care NHS Foundation Trust.

14th Big Health and Wellbeing Day
Gloucestershire Health and Care NHS Foundation Trust, in conjunction with local partner...

Ground Breaking Marks Official Start of Forest Hospital Build
A ground breaking ceremony has been held to mark the official start of building a new community hospital in the Forest of Dean.

Oliver McGowan: NDTi publishes final evaluation report
During 2021, Gloucestershire Health and Care NHS Foundation Trust formed one of four national...

Healthcare Support Worker Week celebrated across the Trust
Our healthcare support colleagues are a critical part of our workforce. Put simply, we could not...
Trust celebrates Armed Forces Week with Defence ERS Silver Award
This week (20-26 June) we're celebrating Armed Forces Week and Armed Forces Day (Saturday 25...

Paul Roberts Announces Plan to Retire
Paul Roberts has taken the decision to retire as our Chief Executive at the end of March 2023. He...

Parliamentary Award for Eating Disorders Lead Sam
A clinician from Gloucestershire Health and Care NHS Foundation Trust has won The Lifetime...
Visiting Restrictions Lifted Today
Visiting restrictions lifted from today

Monkeypox
Monkeypox is a rare infectious disease, but there are a number of cases in the UK. That number is...
Wotton Lawn Hospital: A great place to work
Wotton Lawn Hospital is an 88-bed acute mental health hospital located in the heart of Gloucester....

Dementia Action Week starts on Monday 16 May
Colleagues will be out and about across Gloucestershire for events and awareness raising as part...

Our Experts by Experience
Experts by Experience are people who have personal knowledge of our services, either through their...

End of Life Property Bags for Dying Matters Week
If you know your feed-dogs from your bobbin, your tacking from your frogging, then the Trust would...
Nominations open to join Trust’s Council of Governors
Nominations are now open for you to join our Council of Governors. Our Council needs the following...

Working with the Prince’s Trust to recruit new talent
Our Apprenticeship and Widening Access Team are delighted to be involved with the One...
Notice of Election – Council of Governors
An election will be held for five public vacancies on our Council of Governors. There is one...

Easter Health advice and Pharmacy Opening Times
Plan ahead for a healthy and happy Easter The NHS in Gloucestershire is urging people to keep...

Farewells for Cirencester Matron Linda
Farewells are beginning for Linda Edwards, Matron at Cirencester and Fairford Hospitals, who is...

Community diabetes service receives ‘gold standard’ seal of approval
Our Community Diabetes Service is celebrating the news that its patient education programme has...

Local artists create mural for launch of On Your Mind Glos
Local artists have used street art to mark the launch of On Your Mind Glos and to help raise...

NHS campaign to support survivors of sexual assault & abuse
The NHS has today launched a new campaign to raise awareness of sexual assault referral centres (SARCs) – specialist NHS services that offer specialist practical, medical and emotional support 24/7 to anyone who has been raped, sexually assaulted or abused.

Children’s Mental Health Week – 7-13 February 2022
It’s Children’s Mental Health Week 7-13 February 2022 and we’re taking the opportunity to raise awareness of the support available if you feel you or they need it.

Volunteers add 175 trees to Cirencester hospital grounds
Many thanks to the friendly people at Moore Allen & Innocent who are at Cirencester Hospital today (Thursday 3 Feb) to add some life to the grounds.

Team of the Week – Charlton Lane Hospital
Charlton Lane is based in the spa town of Cheltenham and provides specialist assessment, treatment...

Team of the Week – Wotton Lawn Hospital
Our Team of the Week is Wotton Lawn Hospital in Gloucester! Wotton Lawn Hospital is a mental...

Air conditioning among upgrades at Cirencester Hospital
A series of upgrades have been carried out at Cirencester Hospital through 2021. Coln and Windrush...

Elaine braves the shave in aid of Sue Ryder
Cheltenham and District Nurse Team Lead Elaine Pratten rang in the New Year with a brave new look...

Digital coconut shy wins RITA award for Tewkesbury Hospital
A digital coconut shy contest organised at Tewkesbury Hospital has won staff there a bronze medal...

Plans for £65k allotment project outlined
For years the Montpellier allotment and green space at Horton Road, Gloucester, has provided an...
Tewkesbury MIIU – Temporary Closure
The Minor Injury and Illness Unit in Tewkesbury will be temporarily closed from 8pm on Sunday 19...
Team of the Week – IAPT Team
Our Team of the week is, for the second time this year, our outstanding Improving Access to...

Team of the week: Child and Adolescent Mental Health Services
Our *Team of the week* is our incredible Child and Adolescent Mental Health Services (CAMHS) Our...

Raising awareness of birth-related trauma
Colleagues at Gloucestershire Health and Care NHS Foundation Trust and midwives from...

Better Care Together Awards Celebrate Success
Our annual Better Care Together awards took place virtually - to celebrate the dedication and...

Team of the week – Facilities Team
Our *Team of the week* is our fantastic Facilities team. We have over 200 staff working in our...

Today is World AIDS Day
Thirty-three years ago, 1st December was designated an international day dedicated to raising the awareness of the HIV/AIDS pandemic and remembering those lost to the disease. We have come a long way since then, but there is still more we can do to support ending AIDS.
Police and Crime Commissioner visits Hope House SARC
Hope House SARC received a virtual visit yesterday (Friday 26 November) from Gloucestershire's...

Christmas home safety tips
Our Gloucestershire Home Safety Check Scheme team is getting into the festive spirit and sharing...

Team of the Week: Integrated Community Teams
Our Recruitment team has chosen our Integrated Community Teams (ICTs) as our *Team of the Week* -...

Notice of Election: Council of Governors
Gloucestershire Health and Care NHS Foundation Trust gives notice that it will hold elections to the Council of Governors

Psychological Professions Week, 15 – 19 November 2021
This week (November 15 – 19) we are celebrating and showcasing our amazing psychological...

Team of the week – Practice Education Service
Our *Team of the Week* is our Practice Education Service who, with the support of teams and...

Team of the Week – Eating Disorders Service
Our *Team Of The Week* is our outstanding Eating Disorders Service which provides assessment and...

Moving and Handling Team wins Innovation Award
The Trust’s Moving and Handling Team is celebrating after scooping a national innovation award for...

Apprentices enjoy awards success
We enjoyed a hugely successful night at the Gloucestershire Live Apprenticeship Awards on...

Legs Matter Week 2021
Legs Matter Week – an annual celebration which aims to highlight best practice in leg care and early detection, as well as promote the ‘well leg’.

World Mental Health Day – 10 October
World Mental Health Day is led annually by the World Health Organisation, and is aimed at raising awareness of mental health issues.

Team of the Week – IAPT (Let’s Talk) team
Our Team of the week is our incredible Let’s Talk - Improving Access to Psychological Therapies...
Team of the Week: Integrated Community Teams
Our *team of the week* is our Integrated Community Teams (ICTs) who bring together community...
International Nurses Welcomed to Trust
An international recruitment drive has led to 40 new nurses joining our Trust. The nurses, who are...

Team Of The Week – Crisis Resolution and Home Treatment Team
This week our *Team Of The Week* is our outstanding Crisis Resolution and Home Treatment Team!...

Stroke Unit at Vale highly commended by Community Hospital Association
Vale Hospital in Dursley has been highly commended by the Community Hospitals Association (CHA)...

AHPs Day 2021
Celebrating our Allied Health Professionals October 14th marks national AHPs Day - a day to...

World Suicide Prevention Day – 10 September 2021
We're raising awareness of suicide and suicide prevention as part of World Suicide Prevention Day...

New Chief Operating Officer for Trust
Following a comprehensive national recruitment process, supported by NHS Executive Search, we are...

Notice of Election – Council of Governors
Gloucestershire Health and Care NHS Foundation Trust gives notice that it will hold elections to the Council of Governors

Team of the week: Post-COVID Syndrome Assessment Service
Our Team of the week is our incredible Post-COVID Syndrome Assessment Service – they are a new...

Team of the Week: Let’s Talk (IAPT)
Our Team of the Week is the Let's Talk team, also known as Improving Access to Psychological...

Coln Ward Officially Named South West Award Winners
Coln Ward, from Cirencester Hospital, was officially named the South West winners in the NHS...

Team of the Week: Recovery Team
Our Team of the Week is our amazing Recovery Team They provide a comprehensive community...

Tewkesbury Hospital receives award for Covid response
A brilliant collective response at Tewksbury Hospital to the Covid pandemic has been formally...

Team of the Week: Facilities Team
Our Team of the Week is our incredible Facilities Team – they’ve worked tirelessly for us over the...

Team of the Week: Health Visiting
Our team of the week is our Health Visiting Service - they support families with young children,...
Team of the Week: Mental Health Intermediate Care Team (MHICT)
This week our Team of the Week is Reablement and Home First. The reablement teams are part of the...

We’re celebrating 10 years of our ESD team
The Stroke Early Supported Discharge Team (ESD) was set up 10 years ago in 2011 to enable people...

Team of the Week: Children & Young People’s Services
This week, our team of the week is our Children & Young People’s Services who offer specialist...
Trust awarded Veteran Aware status
We are delighted to announce that Gloucestershire Health and Care NHS FT has been named a Veteran...

Better Care Together – New Strategy Launched by Trust
A new five-year strategy has been officially launched by the NHS Trust which provides community...

Team of the Week: Improving Access to Psychological Therapies (IAPT) Service
Our Team of the Week is our Improving Access to Psychological Therapies (IAPT) service. Find out more about the team, including current job opportunities.
Join Our Team: Estates Team
Find out more about Estates Team, including current job opportunities available within the team.

HRH The Princess Royal Visits Trust
HRH The Princess Royal has spoken to colleagues from our Trust about their work throughout the...

Administrative Professionals Day: Jovelyn Masters
Jovelyn Masters, Personal Assistant to Associate Director of Patient Safety and Learning, talks about her experience of working at GHC.
Administrative Professionals Day: Jon Allard
As part of our celebration of Administrative Professionals Day, Jon Allard, ICT Business and Project Lead, talks about his experience of working at GHC.

Administrative Professionals Day: Evie England, Apprentice Learning and Development Administrator
Evie England, Apprentice Learning and Development Administrator, shares her professional experience in celebration of Administrative Professionals Day.

Maternal Mental Health Care Expands in Gloucestershire
Mental health care and treatment for new, expectant and bereaved mothers in Gloucestershire is...

Team of the Week: Health Visiting Service
This week, find out more about our Health Visiting Service including current job opportunities.

Get involved at the Big Health Check day!
Health and wellbeing event for people with learning disabilities

Team of the Week: Estate and Facilities Teams
This week, our team of the week is our Estates and Facilities Teams, whose responsibility it is to...

Team of the Week: Integrated Community Teams (ICTs)
Our team of the week is our Integrated Community Teams (ICTs). Find out more about the team and what they do., plus current job opportunities.

Life As An Apprentice: Lauryn’s Story
MHICT West Therapy Administrator, Lauryn Kiera Hill, shares her apprenticeship experience.
10 Common Myths About Apprenticeships That Aren’t True
As part of National Apprenticeships Week 2021, the Apprenticeships team have gathered together some interesting myth-busting facts about apprenticeships and what it’s like to be an apprentice.

Life As An Apprentice: Sam’s Story
I started my apprenticeship in 2020 with the IT department based at Edward Jenner Court! This was...

LGBT History Month 2021
February marks the beginning of LGBT History Month 2021, an annual month-long celebration of the LGBT+ community and a time that is used to raise awareness of issues facing lesbian, gay, bisexual, transgender people.

Be Well Gloucestershire: Improving access to support in the county
A new campaign is being launched to encourage people across Gloucestershire to ‘Be Well’ and...

Team of the Week: Perinatal Mental Health team
This week, we’re focusing on our Perinatal Mental health team, who provide care and treatment for women living in Gloucestershire before, during, after their pregnancy.

Temporary Closure of Tewkesbury Minor Injury and Illness Unit – Updated Friday 8th January 2021
The Tewkesbury Hospital Minor Injury and Illness Unit (MIIU) will be closed from 8pm on Sunday 10th January due to operational pressures and the need to direct our resources elsewhere.

Apprenticeship Awards 2021
As part of National Apprenticeship Week 2021, the Apprenticeships team is excited to host a pre-recorded award ceremony, recognising and celebrating the achievements of our current and recently completed apprentices.

Team of the Week: Children in Care team
This week, we’re focusing on our Children in Care Team, whose aim it is to promote and look after the health of children who are in care.
Gloucestershire Christmas Pharmacy Opening Hours
Over the Christmas and New Year period pharmacy opening hours across Gloucestershire will be different, more information about opening hours can be found here.

More than half of us are worried about a loved one’s mental health this Christmas
A survey of over 2,000 UK adults by the Mental Health Foundation found that while 42 percent of people are feeling hopeful, happy or excited about the festive season, 27 percent of adults in the South West are feeling anxious or stressed.

Team of the Week: Estates and Facilities Teams
This week, we’re focusing on our Estates and Facilities Teams. Find out more about the teams, including current job opportunities.

Temporary Closure of Vale Minor Injury and Illness Unit – Updated Wednesday 16 December 2020
The Vale Minor Injury and Illness Unit, near Dursley, will be temporarily closed from 6pm on Sunday 13 December for operational reasons.

Make sure the present you are giving this Christmas is not COVID-19
Health and care leaders in Gloucestershire are urging people to approach the festive period with...

Team of the week: CYPS Immunisation Team
Our Team of The Week this week is our Children and Young People Service (CYPS) Immunisation Team.

Tewkesbury Hospital announced a joint winner in the Community Hospital Association (CHA) annual Innovation and Best Practice Awards.
Tewkesbury Hospital received an early Christmas present after being announced a joint winner in the Community Hospital Association (CHA) annual Innovation and Best Practice Awards.

Vaccinate and protect your child against flu this winter
This year, more than ever, it is really important parents help protect their children against the ‘double danger’ of flu and coronavirus by ensuring they have their flu vaccination.

Team of the Week: Learning Disability Inpatient Services
Our Team of The Week this week is our Learning Disability Inpatient Services based at Berkley...

Team of the Week: Eating Disorder Service
Our Team of The Week this week is our Eating Disorder Service, operating from the Brownhill Centre, Cheltenham.

UK Disability History Month 2020
UK Disability History Month (UKDHM) is an annual event that is designed to focus on the history of disabled people’s fight for equality and human rights.

Gloucestershire Health & Care NHS Foundation Trust Awarded In NHS Parliamentary Awards 2020
Gloucestershire Health & Care NHS Foundation has been awarded in the regional round of the NHS...

Working In Infection Control And Studying At University, All Through A Pandemic
Infection Control Nurse, Amy Barnes, talks about her experiences of working in infection control and studying at university throughout the COVID-19 pandemic.

Armistice Day 2020: Charlton Lane Hospital Poppy Display
In recognition of Armistice Day 2020, patients and staff from Mulberry Ward at Charlton Lane Hospital spent yesterday afternoon making poppies and reminiscing.

Winter Lockdown: Looking After Your Mental Wellbeing
As we head into a second national lockdown in England, we’ve put together ten top tips that be of use when looking after your mental wellbeing over the next month.

Patients encouraged to attend hospital appointments and get the treatment they need
Doctors and other healthcare professionals in Gloucestershire are urging local people to continue to attend their planned and routine appointments in hospital and other NHS settings.
Managing infection control in mental health settings throughout a pandemic
Louise Forrister details the challenges of managing infection control in mental health settings throughout a pandemic.

Public consultation: A new hospital for the Forest of Dean
A Consultation inviting the public to comment on the proposals for the new community hospital in...

Gloucestershire Nurse Awarded MBE
A nurse from Gloucestershire Health and Care NHS Foundation Trust has been awarded the MBE. Sonia...

Managing Memory Together – Online Information Sessions
Our online information sessions are a great way of connecting with others who care for someone...
Annual General Meeting
Our Trust Annual General Meeting (AGM) is being held in September and we'd love you to join us!...
Domestic Abuse and Covid-19 Isolation
An article by Carol Innes, Specialist Safeguarding Nurse – Domestic Abuse, and Penny Humble,...

Lockdown Experiences – Learning Disabilities Week
Dawn and Maisie Dawn and Maisie first met each other in 2009 when they both worked on a Learning...

A GPs Perspective on Lockdown
‘New ways of working’ is a phrase that has been bandied about in General Practice for a few years....

Men and Mental Health in BAME Communities
I was recently asked to write this blog about men in the ‘Black, Asian & Minority Ethnic'...

£375k boost for county mental health services
The county council and Gloucestershire’s NHS have secured £375,000 in extra funding, over three...

Views of Children and Young People to Help Shape Local Mental Health Services
Children and young people, parents, carers and health and social care professionals in...

Mental Health Helpline during Covid-19
A 24-hour a day, seven day a week helpline is now available for anyone in Gloucestershire...

Fire Service and NHS help to increase Covid-19 testing in care homes
Gloucestershire Fire and Rescue Service (GFRS) and NHS staff have teamed up to help care homes in...
Got symptoms that need to be checked out urgently?
Help us help you get the treatment you need. The NHS in Gloucestershire is launching the Help...

Covid-19 Nutrition and Recovery
Jo Sansom, specialist dietitian in our MacMillan Next Steps Service, has written some helpful...
Clare Celebrates 40 Years of Nursing
I started my training to become a Registered General Nurse (RGN) three weeks after my 18th...

Mental Health and Learning Disability Services in Gloucestershire – Changes Due to Coronavirus (Covid-19)
The outbreak of Covid-19 has led to changes in the way some mental health and learning disability...

International Women’s Day
International Women's Day 2021 In celebration of International Women's Day 2021, we interviewed...

Coronavirus Update
The NHS in Gloucestershire and Public Health England (PHE) are well prepared for outbreaks of new...

Jessica’s Nursing Story
Jessica Blakeman is Clinical Systems Development Lead in the Clinical Systems Team at...

Better Care Together – Developing Our Trust Priorities
We are delighted to be presenting our 6th Better Care Together event where we are inviting our...

Gloucestershire cervical screening project wins national award
A project in Gloucestershire aimed at improving access to cervical smear tests for women with...

Become a Community Mental Health Nurse
Community Mental Health services in Herefordshire and Worcestershire are being transformed. As one...

Have your say in the Herefordshire and Worcestershire Mental Health Strategy
Following on from the successful engagement sessions in October 2019, the Clinical Commissioning...

Alison’s Nursing Story
Alison Curson, Head of Nursing and Quality, Gloucestershire Health and Care NHS Foundation Trust,...

Worcestershire NHS Trust to run Herefordshire mental health and learning disability services
Worcestershire Health and Care NHS Trust will take over responsibility for the delivery of...
MBE for Jane Melton
A senior allied health professional from Gloucestershire Health and Care NHS Foundation Trust has...

Ed’s biography documents first leg of his mental health journey
Expert by Experience, Ed Boait, has turned published author with the release of his first book –...

National award win for innovative work around patient data
Gloucestershire Health and Care NHS Foundation Trust’s innovative work to understand the impact...
Norovirus and Flu Information for Visitors
We have confirmed cases of patients with flu at Cirencester Hospital, and norovirus at the Dilke,...

Trust Signs Armed Forces Corporate Covenant
Gloucestershire Health and Care NHS Foundation Trust (GHC) has affirmed its support to the armed...

Severn and Wye Recovery College Graduation 2019
Famed as being the seat of learning for Harry Potter and his fellow Hogwarts alumni, Gloucester...
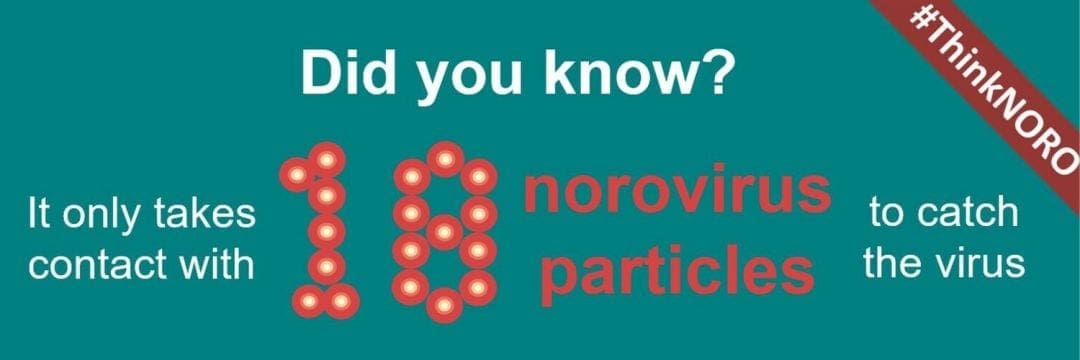
Play your part this winter to stop the spread of Norovirus in the South West – just Think NORO
We can all play a role in stopping the spread of this unpleasant infectious bug Alcohol hand gels...

Melanie Triumphs at Apprenticeship Awards
Senior Community Health Care Support Worker Melanie Woodman has been crowned Healthcare Apprentice...

Trusts to Merge on 1 October
The two NHS trusts providing community mental health, physical health and learning disability...

Trust Helps Celebrate 100 Years Of Learning Disability Nursing
A special event took place at the Churchdown Centre yesterday to mark a century of learning...

Forest of Dean Community Hospital Citizens' Jury
Following the decision of Gloucestershire Care Services NHS Trust and NHS...
Sarah’s Story – PTSD
As part of Mental Health Awareness Week, we are sharing stories of how people have benefited from...
Karen’s Story – Living With OCD
As part of Mental Health Awareness Week, we are sharing stories of how people have benefited from...

Digital Therapy Now Available Through Let’s Talk
If you’re experiencing stress, anxiety, depression or similar issues, there’s now a new way of...

School immunisations programme boosts flu vaccination rate
Flu immunisation rates amongst young children in Gloucestershire soared this winter thanks to...

What matters to you? Supporting you in your community
We are running an event (flyer attached here) where we want to hear from local people about...

Find out about Macmillan Next Steps on BBC Radio Gloucestershire
Listen to Clare Lait, Specialist Community Physiotherapist, talk about the...

#Handitback: Help us to help others by returning your equipment
In Gloucestershire we have a campaign to get any equipment with a GIS Barcode that is unused...

Be on the Ball About Mens Mental Health
Be on the ball about men’s mental health

New Eating Disorders Support Group
New Eating Disorders Support Group

